In a groundbreaking study set to reshape our understanding of pediatric health, a team of researchers led by Moeremans and colleagues has delved into the intricate relationship between Body Mass Index (BMI) and liver fat in children. With alarming rates of obesity among younger populations, this research spotlights a pressing health concern and emphasizes the critical role of early diagnostic techniques. Using ultrasound-derived fat fraction (UDFF) to measure liver fat, the study offers insights that could herald a new era in child health assessment and intervention strategies.
The significance of understanding liver fat in children cannot be overstated, particularly as childhood obesity continues to ascend globally. The liver is a crucial organ in metabolism, and its health is paramount for overall well-being. Excess fat in the liver can lead to conditions such as fatty liver disease, which can progress to more severe liver complications. This research investigates how BMI, a traditional measure of body fat based on height and weight, correlates with liver fat levels, presenting a more complex picture of children’s health than previously acknowledged.
Traditionally, pediatric obesity assessments have relied heavily on BMI. This metric has served as a straightforward method to gauge weight status; however, its limitations are evident, especially in pediatric populations. For instance, BMI does not differentiate between fat and lean mass, potentially masking the true health risks associated with excess fat. The research by Moeremans et al. ventures beyond this conventional approach, integrating UDFF, a more nuanced and accurate method of measuring liver fat composed mostly of triglycerides, which are indicative of metabolic risk.
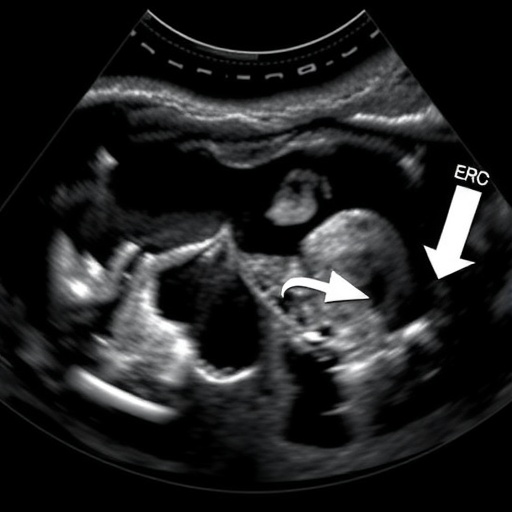
Utilizing UDFF, the researchers collected data from a diverse cohort of children, enabling a thorough analysis of the relationship between BMI and liver fat. By examining these variables collectively, the authors sought to unveil patterns previously overlooked in smaller studies. The research also underscores the importance of non-invasive techniques, such as ultrasound, which holds promise for widespread clinical application in evaluating children’s metabolic health without subjecting them to potential harms of invasive procedures.
The results of this comprehensive study reveal some surprising correlations. A direct link was established between elevated BMI and increased liver fat, validating concerns that higher body mass correlates with poorer liver health in the pediatric population. However, the study also emphasizes the heterogeneity among children; not all children with high BMI exhibit the same levels of liver fat. This variation points towards a multifaceted interplay of genetic, environmental, and lifestyle factors that influence metabolic health, highlighting the need for tailored interventions.
Moreover, Moeremans and colleagues addressed a remarkable phenomenon related to the distribution of fat within the body. While BMI generally serves as a useful proxy for overall body fat, this study illustrates that fat localization is more critical than quantity alone. Children who may be of normal weight could still harbor significant liver fat if their body composition—specifically visceral versus subcutaneous fat—tilts in an unhealthy direction. These findings call into question the effectiveness of relying solely on BMI in determining children’s health risks and emphasize the necessity for more comprehensive screening measures.
As the prevalence of liver-related diseases in adults continues to rise drastically, the research advocates early intervention strategies starting from childhood. The overburden on healthcare systems resulting from untreated childhood obesity and its associated complications underscores the urgency of this knowledge. Early identification through techniques such as UDFF could allow healthcare providers to implement preventive measures tailored to at-risk children, ultimately shifting the paradigm toward proactive health management rather than reactive treatments.
Another point of discussion is the broader implications of this research on pediatric healthcare practices. It signals a shift towards a more integrated model of health assessment, where traditional metrics are complemented by advanced imaging and diagnostic tools. Medical professionals may need additional training to interpret these new data effectively, emphasizing the importance of continued education in pediatric health.
As we navigate the challenges posed by rising childhood obesity rates, public health initiatives aimed at promoting healthy lifestyle choices become increasingly pertinent. This study serves as a timely reminder of the importance of addressing dietary habits and physical activity among children. Alongside clinical interventions, community-focused strategies that foster healthy environments can aid in mitigating the risk of obesity and its associated health complications.
Future research directions suggested by this study include exploring the genetic factors contributing to variations in liver fat beyond BMI. Understanding these genetic predispositions could help in crafting personalized health strategies tailored to individual needs. Additionally, longitudinal studies tracking children over time would provide valuable insights into the causal pathways connecting body composition and metabolic health outcomes.
In summary, the exploration of the relationship between BMI and liver fat in children by Moeremans and colleagues is a pivotal step forward in pediatric healthcare. As the study reveals, a collaborative approach, incorporating advanced diagnostic tools alongside traditional measures, can equip healthcare providers with a deeper understanding of children’s health. With rising rates of obesity-related health issues, this research not only highlights the magnitude of the problem but also illustrates the potential for innovative solutions that could prevent serious consequences later in life.
While the findings present a concerning picture, they also offer a glimmer of hope through early intervention and expanded health assessments tailored to the pediatric demographic. By embracing comprehensive approaches to health and prioritizing preventive care, we can steer future generations towards healthier lifestyles and improved health outcomes.
Ultimately, as this pivotal research unfolds, it invites a re-examination of how we assess, intervene, and nurture the health of our youngest populations—laying the groundwork for a healthier future. With ongoing analysis and robust engagement from the medical community, there stands a good chance that we can combat the rising tide of obesity and its consequences in children, one insightful study at a time.
Subject of Research: Association between Body Mass Index (BMI) and liver fat in children.
Article Title: Exploring the association between BMI and liver fat in children: a study using ultrasound-derived fat fraction (UDFF).
Article References:
Moeremans, M., Barth, R.A., Zalcman, M. et al. Exploring the association between BMI and liver fat in children: a study using ultrasound-derived fat fraction (UDFF).
Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06493-y
Image Credits: AI Generated
DOI: 23 December 2025
Keywords: Pediatric health, BMI, liver fat, childhood obesity, ultrasound-derived fat fraction, metabolic health, non-invasive diagnostics.
Tags: BMI limitations in pediatric healthBody Mass Index and liver fat correlationchildhood obesity health concernsearly diagnostic techniques for obesityfatty liver disease in childreninnovative child health assessment methodsliver fat measurement techniquesliver health in childrenmetabolic health in childrenobesity intervention strategies for childrenpediatric obesity researchultrasound-derived fat fraction