In a groundbreaking study published recently in Acta Parasitologica, researchers have reported the absence of mutations associated with artemisinin resistance in the Plasmodium falciparum Kelch 13 (K13) propeller domain gene across diverse regions of Iran. This finding arrives at a critical juncture in the global fight against malaria, especially considering the widespread use of artemisinin-based combination therapies (ACTs) as frontline treatment against Plasmodium falciparum, the deadliest malaria parasite species.
The K13 gene has been identified as a molecular marker for artemisinin resistance, a serious public health concern that threatens to undermine malaria control efforts worldwide. Since the discovery of mutations in this gene correlating with delayed parasite clearance, the scientific community has closely monitored its prevalence in malaria-endemic regions. Resistance to artemisinin and its derivatives jeopardizes treatment efficacy, necessitating urgent surveillance to inform appropriate interventions.
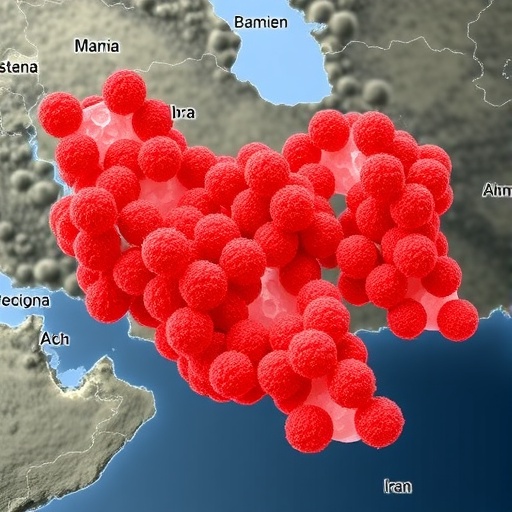
Iran’s situation is particularly notable, positioned geographically where malaria transmission persists in certain southern provinces. The implementation of ACTs has been the standard of care, but until now, the comprehensive genetic surveillance of K13 mutations was lacking. The present study undertook extensive sampling and genetic sequencing efforts to assess whether the widespread ACT application led to the emergence of resistance-conferring mutations within local Plasmodium falciparum populations.
The research team employed rigorous molecular techniques to amplify and sequence the K13 propeller domain from parasite isolates collected from multiple endemic regions over a significant timeframe. Their data encompassed a robust sample size, offering statistically meaningful insights into the genomic landscape of local malaria parasites. Strikingly, the investigators found no evidence of known artemisinin resistance-associated mutations in any of the isolates studied.
This outcome suggests that, despite extensive ACT exposure, Plasmodium falciparum populations in Iran have not developed genetic adaptations conferring resistance through the K13 pathway. Such a development is encouraging and highlights the effectiveness of current malaria management protocols and drug policies in the region. It also underscores the importance of continued vigilance and molecular surveillance to detect resistance at the earliest stages.
Understanding why resistance mutations have not taken hold could inform broader strategies to prevent or delay their emergence elsewhere. The complex interplay between drug pressure, parasite genetics, and transmission dynamics likely contributes to this favorable situation. For example, factors such as reduced malaria transmission intensity and the presence of fitness costs associated with resistance mutations could limit their spread.
Moreover, the study’s findings emphasize the critical role of comprehensive public health initiatives beyond pharmacological interventions. Vector control measures, rapid diagnostic testing, and patient adherence to treatment regimens collectively enhance the durability of current therapies. Iran’s malaria control program appears to effectively balance these components, contributing to the sustained sensitivity of parasites to artemisinin compounds.
The absence of artemisinin resistance-related K13 mutations also provides reassurance for clinicians and patients relying on ACTs as first-line therapy. It supports the continued use of these drugs with confidence in their capacity to clear infections effectively. However, the study’s authors caution that the situation requires ongoing monitoring given the dynamic nature of pathogen evolution and drug resistance development.
Importantly, this research contributes new data to the global map of artemisinin resistance, which has largely been driven by patterns emerging in Southeast Asia and parts of Africa. Evidence from Iran diversifies our understanding of how resistance manifests and spreads geographically, offering a comparative perspective against highly affected regions.
The molecular characterization of Plasmodium falciparum isolates featured in this study utilized cutting-edge sequencing technology, enabling precise detection of both known and novel mutations within the K13 gene. Advanced bioinformatics workflows ensured the reliability of variant calling, a crucial aspect for resistance surveillance where false positives or negatives could skew public health responses.
Additionally, the study design incorporated rigorous sampling methodologies to capture temporal and spatial variation in parasite populations. This approach strengthens confidence that the absence of detected resistance mutations reflects a true epidemiological phenomenon rather than sampling bias or technical limitations.
Given the high stakes involved in managing artemisinin resistance, the findings from Iran advance crucial knowledge for shaping regional and global malaria control policies. They suggest that maintaining integrated malaria control strategies, including robust molecular monitoring, remains vital to preserving the efficacy of ACTs.
Future research directions inspired by this work include exploring other genetic loci potentially involved in resistance mechanisms and evaluating the impact of demographic and environmental variables on parasite genetic diversity. Understanding these nuances will bolster predictive capacities and early warning systems for emergent drug resistance.
In conclusion, the recent comprehensive analysis of the Plasmodium falciparum K13 propeller domain in Iran presents optimistic news for the continued success of artemisinin-based therapies in this region. The nonappearance of mutations linked to artemisinin resistance despite widespread ACT utilization underscores the strength of existing malaria control efforts. However, it also stresses the necessity of sustained investment in molecular surveillance and integrated public health interventions to combat malaria effectively over the long term.
This landmark report not only reinforces the crucial role of genetic epidemiology in infectious disease management but also provides a beacon of hope that with vigilant and coordinated action, the tide of drug-resistant malaria can be impeded. As the global community gears up to eliminate malaria, the insights gained from Iran’s experience offer valuable lessons applicable across endemic countries.
Subject of Research: Detection of Artemisinin Resistance-Associated Mutations in the Plasmodium falciparum K13 Gene Following Widespread Use of Artemisinin-Based Combination Therapy in Iran
Article Title: Absence of Artemisinin Resistance-Associated Mutations in the Plasmodium falciparum Kelch 13 (K13) Propeller Domain Gene Following Widespread Use of Artemisinin-Based Combination Therapy in Iran
Article References:
Mohammadi, S., Forouzesh, F., Mehrizi, A.A. et al. Absence of Artemisinin Resistance-Associated Mutations in the Plasmodium Falciparum Kelch 13 (K13) Propeller Domain Gene Following Widespread Use of Artemisinin-Based Combination Therapy in Iran. Acta Parasit. 71, 5 (2026). https://doi.org/10.1007/s11686-025-01197-7
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11686-025-01197-7
Tags: artemisinin resistance mutationsartemisinin-based combination therapiesgenetic surveillance of malariaglobal malaria control effortsIran malaria research studymalaria treatment efficacymolecular markers for resistancePlasmodium falciparum K13 genePlasmodium falciparum mutationspublic health implications of malariaresistance monitoring in malaria-endemic regionssouthern Iran malaria transmission