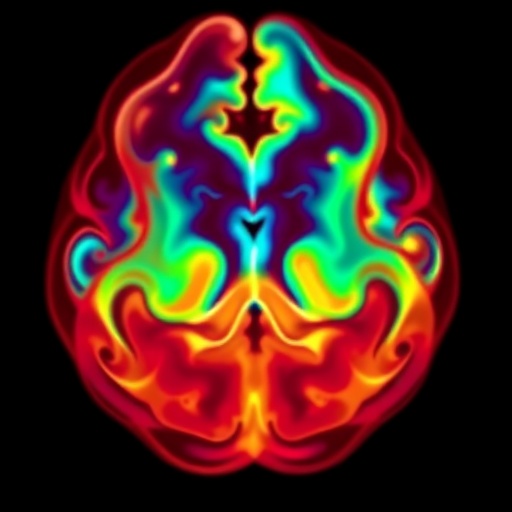
In the intricate landscape of neonatal intensive care, perinatal asphyxia emerges as a formidable adversary, precipitating a cascade of multiorgan dysfunction with devastating consequences. Central to its lethal profile is hypoxemic ischemic encephalopathy (HIE), a condition marked by profound deprivation of oxygen and blood flow to the brain during the perinatal period. The pathophysiology of HIE reflects a complex interplay of ischemia and systemic compromise, with cardiovascular instability playing a pivotal role that challenges existing diagnostic and management paradigms.
At the heart of HIE lies a failure in cerebral autoregulation, a critical mechanism by which the neonatal brain ordinarily maintains steady blood flow despite fluctuating systemic pressures. Asphyxia disrupts this balance, leading to periods of hypoperfusion followed by reperfusion injury, which exacerbates neuronal damage through oxidative stress and inflammation. This derangement extends beyond the brain, manifesting as multiorgan dysfunction syndrome (MODS), where the cardiovascular system reveals its vulnerability most conspicuously. Myocardial ischemia, reduced contractility, and altered vascular tone culminate in hemodynamic instability that complicates therapeutic approaches.
The cardiovascular compromise in infants with HIE is often characterized by hypotension and diminished cardiac output, necessitating the early introduction of inotropic agents to sustain perfusion. Yet, despite the widespread use of inotropes, clinical outcomes remain variable, underscoring the need for refined hemodynamic monitoring and individualized treatment strategies. Traditional markers such as blood pressure and heart rate are insufficiently sensitive to capture the dynamic changes in neonatal circulation during hypoxic insults, prompting a shift toward multimodal monitoring techniques including echocardiography and near-infrared spectroscopy.
Echocardiography offers real-time insights into cardiac function, revealing patterns of systolic and diastolic dysfunction and allowing clinicians to tailor inotropic support accordingly. Studies reveal that myocardial performance indices fluctuate in response to evolving ischemia and reperfusion dynamics, emphasizing the importance of serial assessments. Near-infrared spectroscopy complements this by noninvasively estimating regional tissue oxygenation, thus relating systemic hemodynamics to cerebral oxygen delivery, a crucial determinant in minimizing secondary brain injury.
However, the translation of detailed hemodynamic data into optimized therapeutic algorithms remains challenging. The heterogeneity of HIE patients, driven by variations in the timing, severity, and duration of asphyxial insult, demands nuanced approaches that integrate pathophysiological understanding with bedside diagnostics. Personalized medicine in this domain is evolving, yet it requires robust evidence to delineate which parameters best predict outcomes and guide intervention.
Emerging research also points to the role of systemic inflammation and endothelial dysfunction as mediators of cardiovascular impairment in asphyxia. The inflammatory milieu exacerbates myocardial depression, disrupts vascular autoregulation, and promotes capillary leak, further complicating volume management and inotrope titration. Understanding these molecular pathways opens avenues for adjunct therapies targeting inflammation and preserving endothelial integrity, potentially mitigating hemodynamic collapse.
Another critical aspect is the timing and choice of inotropic agents, which must balance the enhancement of cardiac output against the risks of increased myocardial oxygen consumption and arrhythmogenesis. Dopamine, dobutamine, and milrinone remain mainstays in neonatal care, but their differential effects on systemic and pulmonary circulation require careful consideration, especially in the context of persistent pulmonary hypertension of the newborn (PPHN), frequently concomitant with HIE.
Moreover, therapeutic hypothermia, the current standard of care for moderate to severe HIE, introduces additional hemodynamic challenges. Cooling alters heart rate, vascular resistance, and myocardial metabolism, complicating the interpretation of hemodynamic parameters and the management of cardiovascular support. Tailoring inotropic therapy during hypothermia necessitates an integrated understanding of these physiological shifts to avoid under- or overtreatment.
Beyond pharmacologic management, fluid therapy in infants with HIE necessitates a delicate equilibrium. Hypovolemia impairs perfusion, yet aggressive fluid resuscitation risks precipitating pulmonary edema and exacerbating cerebral injury due to raised intracranial pressure. Volume responsiveness is often unpredictable, reinforcing the utility of bedside echocardiographic assessments and dynamic indices to guide fluid administration judiciously.
Another promising frontier is the incorporation of advanced computational modeling and machine learning tools to synthesize complex hemodynamic data and predict cardiovascular trajectories in HIE infants. Such technologies could enable real-time decision support, improving precision in tailoring interventions and potentially improving neurologic outcomes. Nevertheless, these approaches require rigorous validation in clinical settings.
It is also imperative to recognize the need for standardized protocols that integrate hemodynamic monitoring with neurologic assessment, including amplitude-integrated EEG and neuroimaging findings. Multidisciplinary collaboration between neonatologists, cardiologists, and neurologists is essential to interpret the complex interplay between systemic and cerebral physiology and devise comprehensive care plans.
Despite advances in understanding and technology, significant gaps remain in elucidating the exact hemodynamic alterations in HIE and optimizing therapy. Future research must focus on large-scale, multicenter studies that correlate hemodynamic profiles with short- and long-term neurodevelopmental outcomes. Such endeavors will clarify the prognostic value of hemodynamic parameters and establish evidence-based guidelines for cardiovascular management in this vulnerable population.
In clinical practice, the insights derived from evolving research highlight that managing infants with HIE transcends a one-size-fits-all approach. Instead, it demands an agile, informed strategy that considers the temporal dynamics of ischemic injury, the individual infant’s cardiovascular response, and the multifaceted effects of therapeutic interventions. This paradigm shift has the potential to improve survival while minimizing neurologic sequelae.
Ultimately, addressing the challenges of cardiovascular compromise in HIE calls for a holistic understanding of neonatal physiology, pathophysiology, and therapeutic nuance. Bridging the gaps between bedside assessment, laboratory science, and therapeutic innovation holds promise to transform care paradigms. As research progresses, the integration of sophisticated hemodynamic monitoring with precision medicine approaches heralds a new era in the management of neonatal hypoxemic ischemic encephalopathy.
Subject of Research:
Neonatal hemodynamics and pathophysiological alterations in infants with hypoxemic ischemic encephalopathy following perinatal asphyxia, including cardiovascular compromise and its management.
Article Title:
Hemodynamics in infants with hypoxemic ischemic encephalopathy: pathophysiology and beyond
Article References:
Surak, A., Schmölzer, G.M., McNamara, P.J. et al. Hemodynamics in infants with hypoxemic ischemic encephalopathy: pathophysiology and beyond. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02516-6
Image Credits: AI Generated
DOI: 01 December 2025
Tags: cardiovascular compromise in newbornscerebral autoregulation failurehemodynamic instability in infantsinfant hypoxic-ischemic encephalopathyInflammation in neonatal encephalopathyinotropic agents for perfusion supportmultiorgan dysfunction syndromemyocardial ischemia in neonatesneonatal intensive care challengesoxidative stress in brain injuryperinatal asphyxia effectstherapeutic approaches for HIE