In the relentless pursuit to unravel the complex biological underpinnings of sepsis, a groundbreaking study has emerged from the collaborative efforts of Zhang, Chen, Shen, and colleagues, published recently in Nature Communications. This large-scale multi-omics investigation advances our understanding by identifying novel sepsis subgroups through a sophisticated goal-directed clustering methodology. By integrating diverse molecular data types, the research delineates clear sepsis phenotypes, poised to revolutionize diagnostic precision and therapeutic strategies for this deadly syndrome.
Sepsis, a life-threatening organ dysfunction triggered by dysregulated host responses to infection, remains a formidable clinical challenge worldwide. The heterogeneous nature of sepsis has long frustrated efforts to develop universally effective treatments, as patient responses vary dramatically. Zhang et al.’s approach confronts this heterogeneity head-on by leveraging multi-omics technologies—including genomics, transcriptomics, proteomics, and metabolomics—to capture a multidimensional snapshot of the sepsis pathology.
Central to their study is the innovative employment of goal-directed subgroup identification, a method that simultaneously optimizes for biologically meaningful stratification and clinical relevance. Unlike traditional clustering techniques that rely solely on statistical patterns, this framework integrates prior biological knowledge and specific clinical endpoints to carve out consensus clusters. These clusters are not arbitrary groupings; they reflect distinct molecular signatures and associated clinical trajectories, promising more targeted interventions.
The researchers began by collecting and harmonizing expansive datasets from multiple cohorts, aggregating thousands of molecular features per patient alongside comprehensive clinical metadata. This integration across layers of biological regulation allowed for a holistic examination of sepsis heterogeneity. By imposing stringent quality controls and sophisticated normalization algorithms, the resulting multi-omics compendium became a robust foundation for in-depth computational analyses.
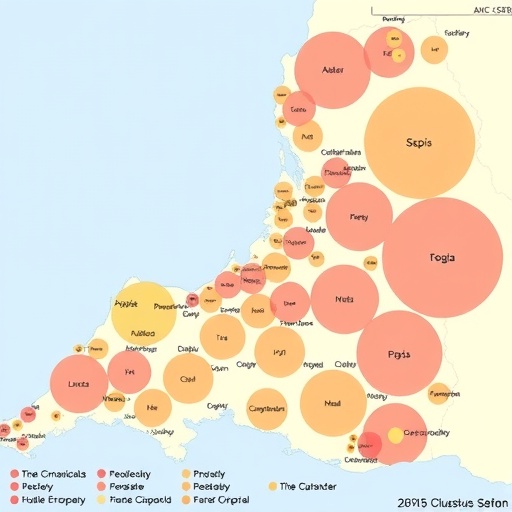
Harnessing advanced machine learning models, the team delineated several highly reproducible sepsis subgroups exhibiting distinct immunological and metabolic profiles. For instance, some clusters were characterized by hyperinflammatory signatures, marked by elevated cytokine levels and immune cell activation pathways. Others demonstrated immunosuppressive phenotypes, with attenuation of antigen presentation and impaired adaptive immune responses. Such molecular heterogeneity mirrors the complex, sometimes paradoxical, immune dynamics observed clinically in septic patients.
In addition to immune patterns, metabolic rewiring emerged as a distinguishing feature among sepsis clusters. Variations in mitochondrial function, energy metabolism, and lipid signaling pathways suggest that metabolic interventions might be tailored to specific patient subsets. The elucidation of these altered biochemical networks sheds light on previously obscured therapeutic targets, opening avenues for precision medicine approaches.
To validate these findings, Zhang et al. performed extensive cross-cohort replication studies and aligned molecular subgroups with clinical outcomes such as mortality, organ failure progression, and response to treatments. The goal-directed clusters exhibited strong prognostic power, outperforming conventional clinical scoring systems. This robust validation underscores the potential for integrating molecular diagnostics into real-world sepsis management workflows.
Excitingly, the study also identified key molecular drivers within each cluster, such as transcription factors and signaling hubs, which may be exploited pharmacologically. These driver molecules serve as biomarkers for patient stratification and as candidates for novel drug development. The rational design of adjunctive therapies informed by such molecular insights could mitigate sepsis’s devastating morbidity and mortality.
Beyond the immediate clinical implications, the study exemplifies the transformative impact of multi-omics integration combined with intelligent clustering algorithms. The interdisciplinary collaboration of bioinformaticians, clinicians, and molecular biologists set a new standard for disease subtyping, applicable far beyond sepsis. This approach embodies the future of systems medicine, where detailed molecular characterization informs decision-making at the bedside.
Importantly, the researchers highlight ongoing challenges, including the need for standardized data collection, greater ethnic diversity in cohorts, and integration of temporal dynamics to capture sepsis progression. Addressing these limitations will be essential to translate molecular subnetworks into actionable clinical tools. However, the current study’s comprehensive methodology lays a profound groundwork for future endeavors.
The publication’s influence is poised to ripple not only through sepsis research but also through the broader biomedical community interested in complex diseases characterized by heterogeneity and multifactorial etiology. It exemplifies how converging technologies and analytical innovations can break down previously inscrutable disease patterns into actionable knowledge.
Moreover, the methodological framework developed by Zhang et al. provides a template for other multi-omics investigations aiming to reconcile biological complexity and clinical needs. As data generation accelerates, this marriage of precision computational methods with biological insight will become increasingly indispensable for medical breakthroughs.
Clinicians and researchers alike are expected to embrace these findings eagerly, anticipating integration into clinical trials and practice. The precision subgroups identified promise to refine patient enrollment criteria, optimize therapeutic regimens, and ultimately improve survival outcomes. Future guidelines for sepsis management may well incorporate molecular stratification as a standard of care.
The study also calls for enhanced collaboration between computational scientists and clinicians, emphasizing the importance of multidisciplinary teams in tackling diseases as multifaceted as sepsis. The synergy between data science and bedside expertise is crucial to harness the full potential of multi-omics insights.
As the field moves forward, the challenge will be scaling these complex analyses to the clinical environment. Automated pipelines, standardized protocols, and cost-effective molecular assays must be developed to facilitate routine implementation. Overcoming these hurdles will allow the profound knowledge gained in research settings to benefit patients on a global scale.
In conclusion, Zhang and colleagues have dramatically advanced our comprehension of sepsis heterogeneity by marrying goal-directed computational clustering with rich multi-omics datasets. Their identification of consensus subgroups with distinct molecular and clinical profiles heralds a new chapter in precision medicine for sepsis. This landmark study not only illuminates novel biological pathways but also sets a transformative course for future research and clinical intervention in critical care.
Subject of Research: Sepsis subtyping through multi-omics integration and computational clustering
Article Title: Deriving consensus sepsis clusters via goal-directed subgroup identification in multi-omics study
Article References:
Zhang, Z., Chen, L., Shen, H. et al. Deriving consensus sepsis clusters via goal-directed subgroup identification in multi-omics study. Nat Commun 16, 10328 (2025). https://doi.org/10.1038/s41467-025-65271-4
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41467-025-65271-4
Tags: advanced clustering methodologiesbiological stratification in sepsisclinical relevance in sepsis studiesconsensus sepsis clustersgenomics and transcriptomics in sepsisheterogeneity of sepsis responsesinnovative approaches in sepsis diagnosismulti-omics sepsis researchproteomics and metabolomics applicationssepsis phenotypes identificationtherapeutic strategies for sepsisunraveling sepsis biology