In an era where rapid advancements in medical imaging technologies are revolutionizing pediatric care, one condition remains a critical focus: pediatric hydrocephalus. This condition, characterized by an abnormal accumulation of cerebrospinal fluid within the ventricles of the brain, can lead to increased intracranial pressure and significant neurological deficits if not diagnosed and treated promptly. A comprehensive review by Elzieny et al. looks deep into the imaging evaluation of ventriculomegaly in emergency settings, providing a pivotal resource for clinicians navigating this challenging landscape.
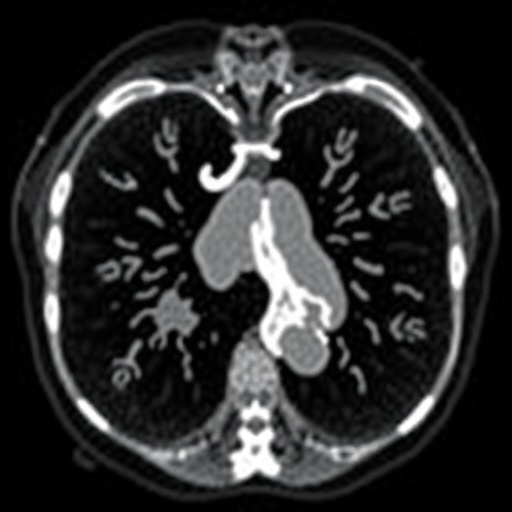
Hydrocephalus, often a congenital anomaly, can also develop secondary to infections, tumors, or traumatic injuries. In the emergency department, the urgent need for accurate and rapid diagnosis is paramount. Given the array of potential underlying causes and the serious implications of delayed treatment, practitioners must rely heavily on advanced imaging techniques. The recent study emphasizes the vital role of modalities such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) in effectively assessing ventriculomegaly.
Ultrasound remains the first-line imaging modality for neonates, particularly due to its portability, non-invasive nature, and lack of radiation exposure. It allows for a real-time assessment of ventricular sizes and configurations, aiding in immediately identifying symptomatic infants. However, limitations such as operator dependency and the window of usability close as the infant grows necessitate the integration of additional imaging techniques.
Computed tomography offers a quick yet potent alternative, especially when a more detailed assessment is required in older infants and children. The ability to analyze bony structures, detect incidental findings, and provide rapid triage capabilities makes CT an indispensable tool in emergency settings. However, the inherent risks associated with radiation exposure in pediatric populations remain a consideration, urging clinicians to weigh the risks and benefits carefully.
Against this backdrop, magnetic resonance imaging emerges as the gold standard for evaluating pediatric hydrocephalus. MRI provides unparalleled detail in visualizing brain anatomy and pathology. The use of contrast agents further enhances the modifiable capacity to delineate between various etiologies of ventriculomegaly and other complications, such as impaired aqueductal flow. However, accessibility issues and the longer duration of MRIs compared to CTs can present logistical challenges in emergency scenarios.
Elzieny et al. underscore the importance of clinical correlation in evaluating images. A thorough history and physical examination must precede any imaging to guide the selection of the appropriate modality and to contextualize findings accurately. Features such as the presence of bulging fontanelles, developmental delays, or neurological deficits can steer investigations and validate imaging interpretations, thereby optimizing patient outcomes.
The study meticulously discusses various conditions mimicking hydrocephalus, such as arachnoid cysts or Dandy-Walker malformation, necessitating a differential diagnosis approach supported by imaging data. Accurate identification of such conditions can alter the management pathway significantly, making proficiency in interpreting pediatric brain scans crucial for emergency physicians and radiologists alike.
Also highlighted is the emerging role of artificial intelligence in interpreting imaging. The integration of AI algorithms can augment diagnostic accuracy, assisting radiologists by identifying subtle patterns that may be overlooked by the human eye. As AI technology continues to advance, its application in emergency pediatric imaging could streamline workflows and improve diagnostic timelines.
However, despite the technological advancements and protocols in place, challenges persist. Variability in institutional practices and accessibility to imaging modalities can create disparity in the timeliness of diagnosis and treatment for pediatric patients. Standardization of care practices and continued education in emerging technologies remain essential to bridge these gaps.
The ramifications of untreated or inadequately managed hydrocephalus extend beyond physical health, influencing long-term cognitive and developmental outcomes for affected children. Continued research, such as that by Elzieny and colleagues, underscores the critical nature of timely and accurate imaging evaluation. As our understanding of the pediatric brain and advancements in imaging techniques evolve, the potential for optimized management and outcomes becomes increasingly tangible.
In defining the future of pediatric hydrocephalus management, collaboration among pediatricians, radiologists, and neurologists is essential. A multidisciplinary approach fosters a comprehensive evaluation that transcends silos and ensures the most effective interventions for young patients. The insights gleaned from this latest research provide a foundation for ongoing discussions and innovations in pediatric hydrocephalus care.
Through the lens of Elzieny et al., we are reminded that behind every imaging study lies a life that can be profoundly impacted by the decisions made based on those images. The quest to improve diagnostics and treatment of pediatric hydrocephalus reflects a broader commitment to safeguarding children’s health, embracing the complexities of pediatric medicine as we strive to offer the best possible care.
In conclusion, the complex interplay of symptoms, imaging modalities, and timely interventions encapsulates the urgency of addressing pediatric hydrocephalus in emergency settings. As we adopt these evolving tools in our clinical arsenal, fostering a culture of continuous learning and collaboration will be key in propelling forward the field of pediatric radiology and enhancing patient outcomes.
Subject of Research:
Pediatric hydrocephalus and imaging evaluation of ventriculomegaly in the emergency setting.
Article Title:
Pediatric hydrocephalus and imaging evaluation of ventriculomegaly in the emergency setting.
Article References:
Elzieny, A., Pace-Soler, E., Thomas, A. et al. Pediatric hydrocephalus and imaging evaluation of ventriculomegaly in the emergency setting. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06397-x
Image Credits:
AI Generated
DOI:
10.1007/s00247-025-06397-x
Keywords: Pediatric hydrocephalus, imaging, ventriculomegaly, emergency setting, ultrasound, CT, MRI, artificial intelligence.
Tags: advanced imaging in pediatric carecerebrospinal fluid accumulationchallenges in diagnosing pediatric conditionscomputed tomography in pediatric emergenciescongenital anomalies in childrenemergency imaging techniques for ventriculomegalyimaging evaluation in emergency settingsmagnetic resonance imaging for hydrocephalusnon-invasive imaging for infantspediatric hydrocephalus diagnosisrapid diagnosis of intracranial pressureultrasound for neonatal ventriculomegaly