In a groundbreaking study poised to influence reproductive medicine, researchers have provided fresh insights into the effectiveness of Progestin-Primed Ovarian Stimulation (PPOS). This method, which has gained traction in recent years, has been critically analyzed for its impact on euploidy rates—the presence of the correct number of chromosomes in embryo development. The study, conducted by Liu, Pan, Wang, and colleagues, specifically examines the effects of micronized progesterone and dydrogesterone compared to traditional GnRH analogues. The findings reveal the nuances of reproductive outcomes across varying age demographics, shedding light on the effectiveness of modern fertility treatments.
The debate surrounding the optimal administration of progesterone during ovarian stimulation has long lingered in the field of reproductive endocrinology. Micronized progesterone and dydrogesterone are both synthetic options designed to mimic the effects of natural progesterone, a hormone critical for preparing the uterine lining for implantation. However, the research has now put these alternatives against the well-established GnRH analogues, determining their respective roles in enhancing euploidy rates during fertility treatments.
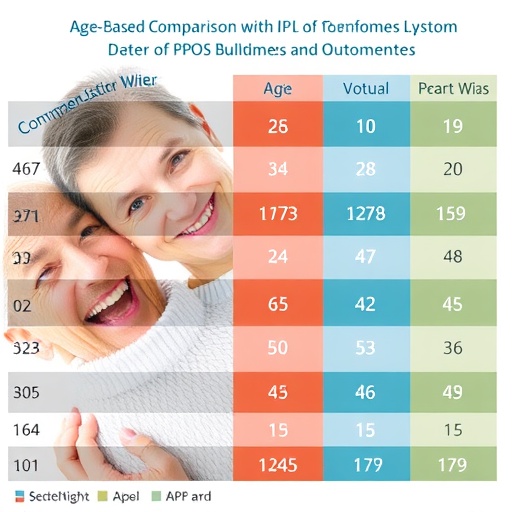
The researchers grouped participants based on age, allowing a detailed evaluation of how age-related factors influence the success of PPOS protocols. Age is a significant determinant of fertility, where older women often face increased risks of chromosomal abnormalities in embryos, leading to lower pregnancy rates and higher chances of miscarriage. By stratifying the data, the study enriches the conversation on age as a core element of fertility planning and treatment efficacy.
The statistical analysis conducted in this study is complex yet revealing. By employing rigorous methodologies to assess euploidy rates across the different treatment regimens, the researchers convincingly illustrate the variations in output. Their analysis demonstrates that while PPOS is a promising avenue for many patients, the nuances of hormone treatment could greatly alter outcomes. This highlights the need for personalized fertility treatment plans where the choice of treatment may be tailored to the specific needs of the patient.
One of the most compelling aspects of this research is the demonstration that not all hormonal treatments are created equal, particularly when administered to patients of varying ages. Younger women may exhibit higher euploidy rates with one form of treatment compared to another. This information could guide physicians in their approach to prescribing fertility treatments and empower women with better-informed choices regarding their reproductive health.
Additionally, as we delve deeper into the implications of this study, it becomes crucial to understand the broader context of fertility treatments available today. While previous studies have often focused solely on the success rates of pregnancy, this new research underscores the importance of genetic viability, pushing the medical community toward a more comprehensive understanding of what successful reproduction entails.
The potential for increased euploidy rates in women using micronized progesterone or dydrogesterone fills a vital gap in fertility treatment knowledge, specifically among age demographics who have typically been underserved. Furthermore, as reproductive technologies continue to advance, aligning hormonal treatments with individualized patient profiles could eventually become standard practice in reproductive clinics.
Adoption of findings from this study would mark a shift towards more nuanced reproductive healthcare. Clinics may begin to integrate these insights into practice by creating specific fertility treatment regimens that acknowledge the biological differences found in aging women. This personalized approach would not only elevate success rates but could also decrease the emotional and financial burdens often associated with fertility treatments.
As the research continues to unfold, it is essential for healthcare providers, policymakers, and patients themselves to engage in discussions surrounding these findings. Education regarding the implications of hormonal treatments must reach a broader audience, empowering women to advocate for personalized care that is informed by scientific evidence.
In conclusion, the study by Liu and colleagues marks a significant contribution to the field of reproductive medicine, especially in its exploration of age-stratified analysis concerning euploidy rates in fertility treatments. It underscores the imperative to tailor fertility interventions to individual patient needs while simultaneously opening avenues for future research. As the landscape of reproductive technology evolves, these insights place us one step closer to revolutionizing how fertility treatments are approached globally.
For those seeking higher success rates in reproductive health, understanding these new findings will be crucial. The medical community stands at a juncture where they must actively digest and apply this information to better serve patients facing the complex challenges of fertility, making the journey to parenthood a more attainable goal for all women, regardless of age.
The quest for optimal reproductive outcomes has taken a significant turn, and as the evidence mounts, we can expect to see influential changes in practices across clinics and hospitals. A brighter future awaits, rooted in tailored treatments that recognize the diverse needs of aspiring parents everywhere.
Subject of Research: Progestin-Primed Ovarian Stimulation (PPOS) and its impact on euploidy rates across different age groups.
Article Title: Age-stratified analysis of euploidy rates in Progestin-Primed Ovarian Stimulation (PPOS) utilizing micronized progesterone or dydrogesterone versus GnRH analogues.
Article References: Liu, R., Pan, X., Wang, Y. et al. Age-stratified analysis of euploidy rates in Progestin-Primed Ovarian Stimulation (PPOS) utilizing micronized progesterone or dydrogesterone versus GnRH analogues. J Ovarian Res 18, 254 (2025). https://doi.org/10.1186/s13048-025-01834-9
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13048-025-01834-9
Keywords: Progestin-Primed Ovarian Stimulation, euploidy rates, micronized progesterone, dydrogesterone, GnRH analogues, fertility treatments, age stratification, reproductive endocrinology.
Tags: age-related fertility outcomeschromosomal health in embryo developmenteuploidy rates in fertilityfertility treatment effectiveness by ageGnRH analogues in IVFmicronized progesterone vs dydrogesteronemodern fertility protocols analysisPPOS techniques comparisonprogestin-primed ovarian stimulationreproductive endocrinology advancementsreproductive medicine insightssynthetic progesterone options