In a groundbreaking new study published in Nature Neuroscience, researchers have uncovered a complex interplay between microglia and astrocytes that profoundly influences Alzheimer’s disease pathology. This study elucidates the nuanced mechanisms by which microglia modulate astrocyte reactivity in response to amyloid-beta (Aβ) accumulation, a hallmark of Alzheimer’s disease (AD). By revealing these intricate cellular dialogues, the research paves the way for innovative therapeutic strategies targeting neuroinflammation and neurodegeneration in AD.
Alzheimer’s disease is characterized by an insidious cascade of pathological events, including the buildup of Aβ plaques and neurofibrillary tangles. Although the involvement of microglia—the brain’s resident immune cells—and astrocytes—the star-shaped glial cells fundamental to neuronal support—has been recognized, the precise nature of their interactions remained elusive. This study provides critical insights into how microglia dynamically regulate astrocyte states in an Aβ-dependent manner, influencing disease progression.
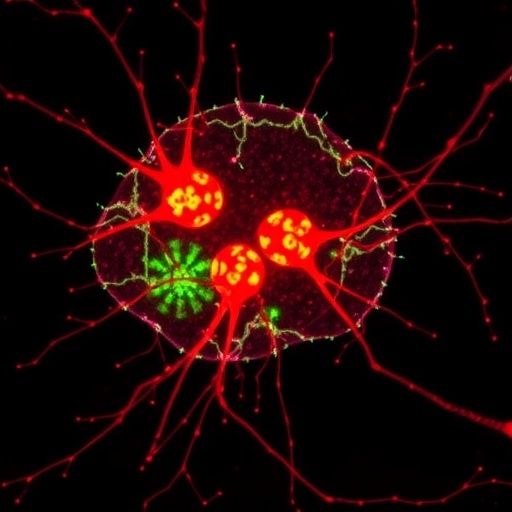
Central to the research is the concept that microglia act not just as independent effectors of neuroinflammation but as regulators of astrocyte behavior, thereby orchestrating a broader glial response to Aβ pathology. The authors utilized a combination of advanced single-cell transcriptomics, in vivo imaging, and functional assays in both mouse models of AD and human brain tissue to dissect the molecular cross-talk between these two glial populations.
Detailed transcriptomic analyses revealed that microglia undergo Aβ-dependent activation states characterized by a distinct gene expression profile. These reactive microglia release a suite of signaling molecules, including cytokines and chemokines, which in turn modulate astrocyte phenotypes. Notably, astrocytes exposed to microglial signals exhibited a shift toward a reactive phenotype characterized by altered calcium signaling, changes in neurotransmitter uptake mechanisms, and a pro-inflammatory secretory profile.
One of the seminal findings of this study is the identification of specific molecular pathways through which microglia influence astrocyte reactivity. The research highlights key receptor-ligand interactions, including those involving TREM2 and complement system components, which mediate the bidirectional communication between these glial cells. This microglia-driven modulation appears to amplify astrocyte response to amyloid plaques, potentially exacerbating synaptic dysfunction and neuronal damage.
These findings challenge the traditionally neuron-centric view of Alzheimer’s disease and emphasize the critical role of glial networks in shaping disease outcomes. By revealing that microglial activity directly sculpts astrocyte behavior, this study underscores the importance of targeting glial communication pathways rather than discrete cellular targets in isolation. Such an approach could yield more effective interventions capable of modulating the neuroinflammatory environment and slowing neurodegeneration.
Furthermore, the authors demonstrate that disrupting the dialog between microglia and astrocytes alters disease trajectory in mouse models. Genetic or pharmacological inhibition of microglial signaling molecules attenuated astrocyte reactivity and mitigated synaptic loss, suggesting that manipulation of this intercellular communication axis can confer neuroprotection. These preclinical findings herald promising translational opportunities for AD therapies.
Importantly, the study also validates these mechanisms in postmortem human AD brain tissue, confirming that the interplay between microglia and astrocytes observed in murine models is conserved in humans. This cross-species confirmation bolsters the relevance of microglia-astrocyte interactions in the human condition and strengthens the translational potential of targeting this pathway clinically.
The research methodology itself reflects a tour de force in modern neuroscience. The combination of single-cell RNA sequencing with sophisticated in vivo imaging allowed the investigators to map the temporal evolution of glial states during disease progression with unprecedented resolution. This approach sheds light on how microglial activation predates and potentially drives astrocytic transformation, framing a chronological sequence of glial dysfunction in Alzheimer’s disease.
This study not only advances our understanding of cellular interplay in AD but also redefines potential biomarkers for disease staging and prognosis. Reactive astrocyte signatures modulated by microglial input may serve as indicators of disease severity or progression, providing new tools for clinical assessment and therapeutic monitoring.
Moreover, the findings suggest that therapeutic strategies modulating microglial activation must carefully balance immune functions. Microglia play essential roles in debris clearance and synaptic pruning; thus, complete suppression risks detrimental side effects. Targeting the mechanisms underlying pathological microglia–astrocyte interactions while preserving physiological functions represents a delicate but crucial therapeutic frontier.
In light of these results, pharmaceutical development efforts could focus on small molecules or biologics that selectively modulate TREM2 signaling or complement pathway activity in microglia to recalibrate astrocyte reactivity. Such precision interventions might mitigate neuroinflammation without broadly suppressing immune surveillance in the central nervous system.
This study exemplifies the evolving paradigm in neurodegenerative disease research, emphasizing the brain’s cellular ecosystem rather than isolated cell types. The intimate, context-dependent communications between microglia and astrocytes unveiled here suggest that neurodegeneration emerges from complex glial networks that can be strategically targeted to restore homeostasis.
As Alzheimer’s disease continues to impose an immense societal burden, discoveries like these offer a beacon of hope by revealing novel cellular targets and mechanisms. Understanding the interplay between glial cells enhances our conceptual framework and opens avenues for innovative treatments aimed at halting or even reversing disease progression.
In conclusion, the work by Ferrari-Souza and colleagues constitutes a paradigm-shifting contribution to Alzheimer’s disease biology. By decoding the molecular dialogue between microglia and astrocytes in the context of Aβ pathology, the study illuminates the dynamic glial landscape driving neuroinflammation and neurodegeneration. Future research building on these findings may transform how the scientific community approaches Alzheimer’s therapeutics, prioritizing nuanced modulation of glial interactions to improve patient outcomes.
Subject of Research: Microglial modulation of amyloid-beta-dependent astrocyte reactivity in Alzheimer’s disease
Article Title: Microglia modulate Aβ-dependent astrocyte reactivity in Alzheimer’s disease
Article References:
Ferrari-Souza, J.P., Povala, G., Rahmouni, N. et al. Microglia modulate Aβ-dependent astrocyte reactivity in Alzheimer’s disease. Nat Neurosci (2025). https://doi.org/10.1038/s41593-025-02103-0
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41593-025-02103-0
Tags: Alzheimer’s disease pathologyamyloid-beta accumulation effectscellular dialogues in Alzheimer’sglial response to neurodegenerationhuman brain tissue studiesmicroglia and astrocyte interactionsmouse models of Alzheimer’s researchneuroimmune interactions in brain healthneuroinflammation in Alzheimer’sregulation of astrocyte reactivitysingle-cell transcriptomics in neurosciencetherapeutic strategies for neurodegeneration