Recent research conducted by Liu, Deng, and Huo et al. has shed light on the impacts of human coronavirus OC43 (HCoV-OC43) infection within human cerebral organoids. This novel approach utilizes engineered brain-like structures to dissect the mechanisms underlying viral pathogenesis in a more physiologically relevant context than traditional cell culture or animal models. HCoV-OC43, a member of the coronaviridae family, is particularly noteworthy due to its historical association with mild respiratory illnesses yet, in specific populations, it can result in severe neurological complications. Understanding how this virus behaves within neural tissues is critical for elucidating its role in both infectious disease and potential neurodegenerative processes.
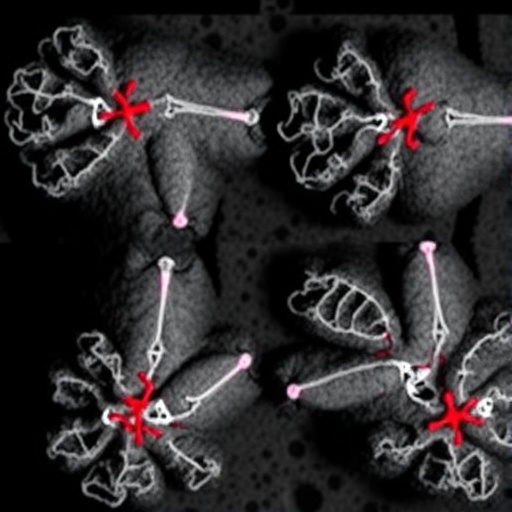
The phenomena of using cerebral organoids—three-dimensional, miniaturized versions of the brain derived from stem cells—has revolutionized the means by which researchers can model human brain disorders. This methodology is pivotal because it allows for the study of viral infections in a human-like environment, where the cellular architecture and microenvironment of brain tissue can be loosely replicated. The findings from the study demonstrate that HCoV-OC43 can effectively enter these organoids and elicit pathological responses, providing a competitive advantage in understanding how this virus can contribute to neurological disorders.
A key aspect that emerged from the research is the differential response of various cell types within the cerebral organoids to HCoV-OC43 infection. Neuronal cells showed varied susceptibility when exposed to the virus, which hints that certain types of neurons may be more vulnerable to the effects of the infection. This cellular heterogeneity may explain why some patients develop neurological symptoms, while others experience predominantly respiratory issues, emphasizing the complexity of host-pathogen interactions at the cellular level.
Furthermore, the organoid model revealed intriguing insights into the inflammatory pathways activated in response to HCoV-OC43 infection. The research documented an up-regulation of inflammatory cytokines and chemokines, indicating that the immune response mounted by the neural tissue can exacerbate the infection effects. This inflammatory milieu can lead to neuronal cell death and contribute to the long-term consequences that viral infections may impose on brain health, a focus of increasing interest among neuroscientists and clinicians alike.
Implications of these findings extend to therapeutic strategies. As the study notes, understanding the molecular pathways activated during infection may help in identifying potential targets for intervention. For example, agents that could dampen the inflammatory response or direct antiviral strategies may offer promising avenues for reducing not only the acute impact of the viral infection but also the risk of long-term neurological decline.
The study’s results are particularly relevant in a world still grappling with the repercussions of the COVID-19 pandemic, as they highlight the necessity of understanding other coronaviruses beyond SARS-CoV-2. With COVID-19 variants continuing to emerge, researchers are keenly aware that historical viruses like HCoV-OC43 could also play undiscovered roles in exacerbating ongoing public health challenges. Thus, investing in this line of research may yield not only immediate clinical applications but also a broader understanding of viral impacts throughout human history.
Another fascinating aspect of the study is its potential to contribute to the development of vaccines and therapeutic interventions targeted explicitly for neurological effects linked to coronavirus infections. By uncovering the specific viral mechanisms and host interactions that lead to neurological manifestations, precise and effective therapeutic strategies could be designed. This could prove to be transformative for treating patients suffering from post-viral syndromes.
Moreover, the work of Liu et al. aligns with a growing body of evidence suggesting that viral infections can trigger neuroinflammatory conditions, and studying coronaviruses within neural contexts opens up avenues for understanding these phenomena. Diseases such as multiple sclerosis and other neurodegenerative disorders might share common threads with viral infections, further necessitating clarity in the pathogenesis of how coronaviruses affect the brain.
The use of cerebral organoids as a platform for studying HCoV-OC43 infection represents a pioneering approach. This study adds to the momentum of using such advanced platforms in virology, especially in understanding how zoonotic viruses adapt to human neural microenvironments. Continuing the research in this direction could unveil various other pathogens’ roles in closing the gap between viral infections and neurodegenerative diseases.
In conclusion, Liu et al.’s study paves the way for future investigations that could unravel the intertwined relationships between coronaviruses, immune responses, and neurodegenerative disorders. As our understanding of viral pathogenesis within the brain evolves, so too does our arsenal for combating the potential long-term effects of these infections. The need for innovative research in this field has never been more critical, especially considering the multifaceted nature of how viruses can affect human health.
In summary, the study invokes a clarion call for heightened awareness and research focus on how even mild viruses, like HCoV-OC43, can lead to severe consequences in human health, particularly concerning the brain. This foundation not only enriches our understanding of infectious diseases but also sets the stage for future therapeutic possibilities that leverage new biotechnologies to address longstanding healthcare challenges.
Subject of Research: Human coronavirus OC43 infection in human cerebral organoids.
Article Title: Human coronavirus OC43 infection in human cerebral organoids: novel insights on pathogenesis and potential therapeutic interventions.
Article References: Liu, J., Deng, Y., Huo, W. et al. Human coronavirus OC43 infection in human cerebral organoids: novel insights on pathogenesis and potential therapeutic interventions.
J Biomed Sci 32, 96 (2025). https://doi.org/10.1186/s12929-025-01193-z
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12929-025-01193-z
Keywords: Human coronavirus OC43, cerebral organoids, viral pathogenesis, neuroinflammation, therapeutic interventions.
Tags: brain organoids researchhuman coronavirus OC43impact of coronaviruses on neural tissuesinfectious disease and neurodegenerationneurological complications of HCoV-OC43OC43 infection mechanismsphysiological relevance of cerebral organoidsstem cell-derived brain modelsthree-dimensional brain tissue modelingunderstanding COVID-19 in brain healthviral infections and brain disordersviral pathogenesis in neuroscience