Scientists at the Keck School of Medicine of USC, operating within the Southern California Superfund Research and Training Program for PFAS Assessment, Remediation and Prevention (ShARP) Center, have unveiled groundbreaking insights into the impact of perfluoroheptanoic acid (PFHpA) on adolescent liver health. PFHpA, a relatively underexplored member of the per- and polyfluoroalkyl substances (PFAS) family commonly described as “forever chemicals” due to their persistence in the environment, has now been linked to a marked increase in risk and severity of metabolic dysfunction-associated steatotic liver disease (MASLD) in obese youths. This revelation, published recently in the prestigious journal Communications Medicine, merges clinical data from a pioneering cohort of adolescents undergoing bariatric surgery with innovative three-dimensional liver organoid models to dissect the pathophysiological underpinnings of PFHpA-induced liver damage.
The investigation arose from the analysis of blood samples collected from 137 adolescents enrolled in the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS), the largest longitudinal study of pediatric bariatric surgery in the United States. Researchers identified that those adolescents exhibiting blood PFHpA concentrations twice as high as their counterparts faced an 80% greater probability of being diagnosed with MASLD. Moreover, these individuals demonstrated more advanced pathological hallmarks, including hepatic inflammation and fibrosis, which are established precursors to cirrhosis, liver failure, and hepatocellular carcinoma. This clinical association was substantiated through meticulous laboratory experiments employing PFHpA doses commensurate with real-world human exposure levels. Using 3D liver spheroids cultivated under controlled conditions, the team delineated how PFHpA disrupts critical biological pathways involving inflammatory signaling cascades, oxidative stress induction, and aberrant lipid metabolism, all converging to propagate hepatic injury. The synergy of patient-derived clinical data with rigorous in vitro modeling enabled the characterization of a unique molecular signature emblematic of PFHpA-mediated hepatotoxicity.
Metabolic dysfunction-associated steatotic liver disease, previously recognized as non-alcoholic fatty liver disease (NAFLD), remains one of the most prevalent hepatic conditions in children and adolescents nationwide, affecting about five to ten percent of this population and exceeding 30% prevalence among those with obesity. Alarmingly, MASLD incidence is climbing, portending severe complications such as type 2 diabetes mellitus and cardiovascular pathology. The identification of PFHpA as a contributory environmental factor exacerbating MASLD progression carries profound implications, especially given the ubiquitous presence of PFAS substances. Owing to their widespread use in consumer goods like food packaging, waterproof apparel, cosmetics, and non-stick cookware, PFAS contamination extends across numerous water supplies throughout the United States. Recent estimates indicate nearly half of all American municipal water systems contain measurable PFAS concentrations, underscoring the pressing public health challenge.
Dr. Lida Chatzi, MD, PhD, the study’s senior investigator and director of the ShARP Center, emphasized the significance of these findings, noting that “PFHpA, despite being less notorious than legacy PFAS such as PFOA and PFOS, likely poses comparable risks to human health.” Her call to action stresses the imperative for comprehensive regulatory frameworks that encompass emerging PFAS compounds alongside well-characterized legacy chemicals. This holistic regulatory approach is necessary to mitigate community exposures that continue unabated amid evolving chemical production landscapes.
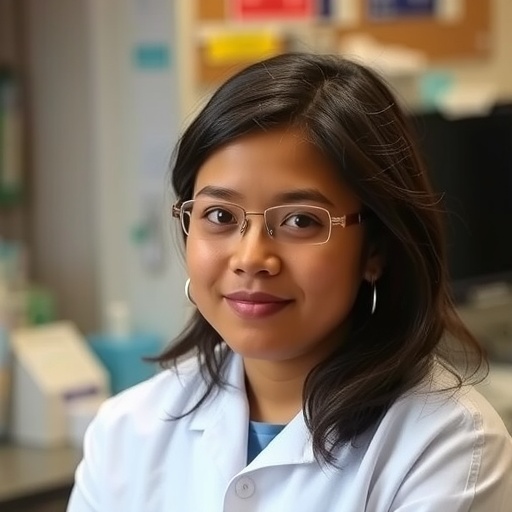
The study’s translational framework exemplifies a robust integration of epidemiology and bench science. Brittney O. Baumert, PhD, MPH, lead author and postdoctoral fellow at USC, highlighted that “our research transcends correlative analyses, leveraging translational methodologies to elucidate the cellular and molecular perturbations induced by PFAS exposure.” By bridging clinical phenotypes with mechanistic data, the team aims to empower precision environmental health efforts that can identify and shield vulnerable groups—especially children and adolescents who bear heightened susceptibilities during critical windows of development.
Complementing this work, co-investigator Ana C. Maretti-Mira, PhD, led the in vitro studies that mapped PFAS activation of intracellular pathways within liver cells. “Decoding these pathways permits the identification of potential therapeutic targets to intervene before PFAS-related liver disease reaches irreversible stages,” she explained. This approach not only advances mechanistic understandings but also opens avenues for clinical interventions aimed at interrupting the progression from early hepatic injury to chronic liver disease.
Embedded within the broader mission of the USC Superfund Research Program, funded by the National Institute of Environmental Health Sciences (NIEHS), this research exemplifies a commitment to deciphering the health impacts of hazardous chemical exposures and translating findings into actionable prevention and policy. The USC team employed state-of-the-art exposomics technologies, including untargeted metabolomics, proteomics, and single-cell transcriptomics, to precisely characterize the molecular footprints of PFHpA exposure. Such sophisticated methodologies enable unprecedented resolution in linking environmental exposures to health outcomes, fostering a new era of precision environmental medicine.
Looking forward, the ShARP Center aims to extend its research to real-world community settings, focusing on the reduction of PFAS exposures through innovative engineering solutions and enhanced public engagement. Efforts will include the development of advanced PFAS remediation technologies, community education initiatives to raise awareness and behavioral modifications, as well as training programs to cultivate the next generation of environmental health scientists and engineers. These comprehensive strategies are integral to advancing precision health paradigms, where interventions can be tailored to individual risk profiles and environmental contexts to more effectively prevent chemical-mediated diseases.
The multi-institutional research team assembled for this study includes experts spanning the University of Southern California, Emory University, Barcelona Institute for Global Health, University of Rhode Island, Mount Sinai Icahn School of Medicine, University of California campuses, Northwestern University, Cincinnati Children’s Hospital Medical Center, Baylor College of Medicine, the National Cancer Institute, Children’s Hospital Los Angeles, and others. This collaborative network underscores the complexity of unraveling environmental health challenges and the necessity of cross-disciplinary expertise.
Funding sources supporting this work encompass a broad sweep of national and international agencies, reflecting the global urgency of addressing PFAS contamination and its health ramifications. These include the NIEHS, the National Institutes of Health (NIH), European Union exposome initiatives such as ATHLETE, California Environmental Protection Agency, and the U.S. Department of Agriculture. The diverse financial backing enables comprehensive research from molecular mechanistic studies to community-engaged interventions, fostering translational impact.
Conflict of interest disclosures reveal that while most authors report no conflicts, a few have consultancy relationships or advisory roles with pharmaceutical companies unrelated to this study, ensuring transparency. Notably, Dr. Bartell and Dr. Chatzi have provided expert assistance in legal cases involving PFAS exposures, reflecting their recognized expertise in this arena.
This landmark study fundamentally shifts our understanding of how lesser-known PFAS compounds like PFHpA contribute to childhood liver disease, a condition with rapidly escalating prevalence and severe long-term consequences. By illuminating molecular mechanisms and championing comprehensive research-to-policy pathways, it paves the way for targeted interventions to safeguard vulnerable youth globally, addressing a critical public health crisis with precision and urgency.
Subject of Research: Lab-produced tissue samples
Article Title: Translational Framework Linking Perfluoroheptanoic Acid (PFHpA) Exposure to Metabolic Dysfunction Associated Steatotic Liver Disease in Adolescents
News Publication Date: 29-Oct-2025
Web References:
Southern California Superfund Research and Training Program for PFAS Assessment, Remediation and Prevention (ShARP) Center: https://sharpcenter.usc.edu/
Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study: https://www.niddk.nih.gov/about-niddk/research-areas/obesity/bariatric-surgery-teens-severe-obesity-study-teen-labs
Communications Medicine article DOI: http://dx.doi.org/10.1038/s43856-025-01168-z
References:
The original peer-reviewed publication in Communications Medicine (Nature Portfolio), along with cited funding grants and participating institutions detailed in the research disclosure.
Keywords: Liver damage, Fatty liver disease, Steatohepatitis, Liver cancer, Chemical pollution, Water pollution, Pollutants, Inflammation, Oxidative stress, Lipid metabolism
Tags: adolescent liver healthbariatric surgery adolescent outcomesMASLD severity and prevalencemetabolic dysfunction in youthobesity and liver diseaseperfluoroalkyl substances studyPFAS environmental impactPFHpA blood concentration effectsPFHpA liver disease riskSuperfund research findingsthree-dimensional liver organoidsUSC Superfund Research Center