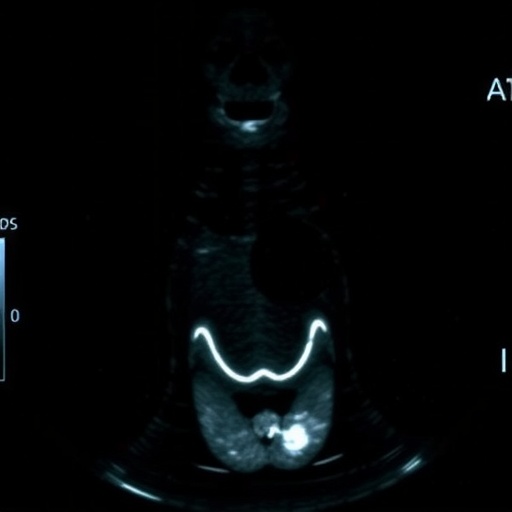
In an era where precision medicine is rapidly advancing, the ability to predict disease progression and tailor treatments accordingly is more critical than ever. A groundbreaking study recently published in BMC Cancer has shed light on a novel predictive tool designed to improve clinical decision-making in papillary thyroid carcinoma (PTC), a common form of thyroid cancer. This tool—a nomogram that integrates both conventional ultrasound (US) and contrast-enhanced ultrasound (CEUS) imaging features—aims to accurately forecast high-volume central lymph node metastasis (HVCLNM), a complication that necessitates careful surgical planning.
High-volume central lymph node metastasis, defined as the presence of five or more pathological N1a metastases, poses significant challenges in managing PTC. Patients presenting with HVCLNM often require a second total thyroidectomy following an initial unilateral thyroidectomy, underscoring the imperative for preoperative identification. Until now, clinicians have faced difficulties in assessing the likelihood of HVCLNM using standard imaging methods, which can lead to suboptimal surgical strategies or delayed treatment adjustments.
The research team, spearheaded by Yan, X., Peng, Q., and Chen, J., compiled a comprehensive dataset comprising 867 patients diagnosed with PTC between May 2021 and May 2024. This cohort was randomly divided into a training group and a validation group in a 7:3 ratio, ensuring robust model development and testing. By fusing conventional ultrasound characteristics—such as tumor size and multifocality—with dynamic imaging data from CEUS, which highlights tumor vascularity and enhancement patterns, the study harnessed multimodal imaging insights to enhance predictive accuracy.
To distill the most predictive features from the imaging data, the researchers employed the Least Absolute Shrinkage and Selection Operator (LASSO) logistic regression method. This approach identified five key variables strongly associated with HVCLNM: tumor size, multifocality, enhancement direction observed in CEUS, peak intensity of contrast uptake, and lymph node status as reported by ultrasound. These factors were then integrated into a statistically rigorous nomogram, which provides individualized risk assessments based on patient-specific imaging profiles.
Performance evaluation of the nomogram demonstrated remarkable diagnostic power. In the training dataset of 607 patients, the model achieved an area under the receiver operating characteristic curve (AUC) of 0.9149, signifying excellent discrimination between patients with and without HVCLNM. The validation dataset, consisting of 260 patients, also confirmed the model’s robustness with an AUC of 0.8768. These figures highlight the nomogram’s potential to reliably identify high-risk patients preoperatively.
Beyond discrimination metrics, the study rigorously assessed calibration, ensuring the predicted probabilities of metastasis closely matched observed outcomes. Decision curve analysis further substantiated the clinical utility of the nomogram, showcasing its net benefit across a range of threshold probabilities and positioning it as a valuable tool for guiding therapeutic decisions. This multilayered evaluation underscores the nomogram’s readiness for real-world application.
The integration of contrast-enhanced ultrasound represents a notable advance in thyroid cancer imaging. Unlike traditional ultrasound techniques that provide anatomic detail, CEUS captures dynamic vascular features—information that is particularly relevant given the angiogenic nature of metastatic lymph nodes. By incorporating enhancement patterns and flow directionality, the nomogram leverages subtle imaging biomarkers that correlate strongly with metastatic burden.
Clinicians managing PTC patients stand to benefit from this predictive model, which can refine surgical planning by anticipating the need for more extensive lymph node dissection. Avoiding unnecessary second surgeries not only reduces patient morbidity and healthcare costs but also streamlines treatment pathways. Moreover, early identification of HVCLNM facilitates more aggressive adjuvant therapies and closer postoperative surveillance, potentially improving long-term survival and quality of life.
The study’s methodological rigor is complemented by its clinical relevance. The large sample size, prospective enrollment period, and balanced training-validation split lend credibility to the findings. Additionally, the use of LASSO regression minimizes overfitting, ensuring the nomogram’s applicability across different patient populations and imaging platforms.
While promising, the study also acknowledges certain limitations. Factors such as interobserver variability in ultrasound interpretation and the generalizability of results to populations with diverse demographic characteristics warrant further investigation. Future research aimed at integrating molecular markers and expanding validation cohorts could enhance the nomogram’s predictive scope.
In summary, this pioneering work establishes a high-accuracy nomogram that synthesizes conventional and contrast-enhanced ultrasound data to preoperatively predict high-volume central lymph node metastasis in papillary thyroid carcinoma. Its implementation could revolutionize patient stratification and personalize surgical approaches, aligning with the broader goals of precision oncology.
As the oncology community continues to embrace advanced imaging and data integration, tools like this nomogram may soon become indispensable components of thyroid cancer management. The convergence of innovative imaging modalities and sophisticated statistical modeling heralds a new chapter in cancer diagnosis and treatment optimization.
With thyroid cancer incidence on the rise worldwide, timely and accurate assessment of metastatic risk is imperative. This study not only addresses a critical clinical gap but also exemplifies the transformative potential of merging imaging technology with predictive analytics.
The translational impact of this research, bridging diagnostic imaging and surgical decision-making, epitomizes the future of cancer care, wherein personalized treatment algorithms improve outcomes while minimizing unnecessary interventions.
In the context of evolving therapeutic landscapes, particularly in endocrine oncology, the capacity to finely stratify patients based on metastatic risk aligns with efforts to tailor treatment intensity and follow-up strategies, reducing overtreatment.
Ultimately, the nomogram developed by Yan and colleagues stands as a testament to the promising horizon of computer-assisted diagnostic tools enriched by multiparametric ultrasound imaging, offering a beacon of hope for patients navigating the complexities of papillary thyroid carcinoma.
Subject of Research: Development of a predictive nomogram integrating conventional and contrast-enhanced ultrasound imaging features to assess high-volume central lymph node metastasis in papillary thyroid carcinoma.
Article Title: A nomogram based on conventional and contrast-enhanced ultrasound for predicting high-volume central lymph node metastasis in papillary thyroid carcinoma.
Article References:
Yan, X., Peng, Q., Chen, J. et al. A nomogram based on conventional and contrast-enhanced ultrasound for predicting high-volume central lymph node metastasis in papillary thyroid carcinoma. BMC Cancer 25, 1529 (2025). https://doi.org/10.1186/s12885-025-15023-w
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-15023-w
Tags: challenges in thyroid cancer surgeryClinical decision-making in cancer treatmentcontrast-enhanced ultrasound in oncologyhigh-volume central lymph node metastasispapillary thyroid carcinoma imagingpredicting thyroid cancer metastasispredictive tools in precision medicinepreoperative assessment of thyroid cancersurgical planning for thyroid cancerthyroid cancer patient managementthyroid cancer research and innovationultrasound nomogram for thyroid cancer