In a groundbreaking advancement for neuro-oncology, researchers have unveiled a novel predictive model capable of determining the consistency of pituitary neuroendocrine tumors (PitNETs) prior to surgical intervention. Utilizing multiparametric magnetic resonance imaging (mpMRI) coupled with sophisticated radiomics analysis, this multicenter study promises to redefine preoperative planning by offering unprecedented insights into tumor texture and composition through non-invasive imaging techniques.
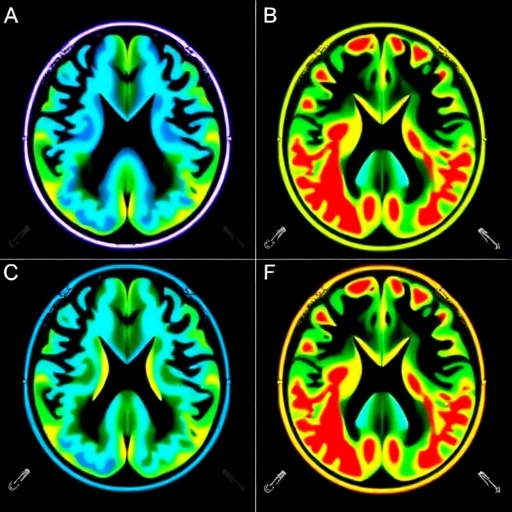
The investigation centers on the clinical imperative to distinguish between soft and hard PitNET consistency, a factor historically reliant on intraoperative tactile assessment. Accurate preoperative prediction of tumor consistency holds immense potential to tailor surgical strategies, minimize operative risks, and improve patient outcomes. Capitalizing on mpMRI, this study leverages the rich imaging data derived from sequences including T1-weighted imaging (T1WI), T2-weighted imaging (T2WI), and contrast-enhanced T1-weighted imaging (CE-T1) to construct a multidimensional radiomic profile reflective of underlying tumor heterogeneity.
Drawing on a robust retrospective cohort of 137 patients who underwent preoperative mpMRI, the research stratified tumor consistency based on detailed neurosurgical records. The patient data were divided into a large training set and a carefully curated internal validation set to ensure rigorous model development and initial performance verification. Radiomics features extracted from both two-dimensional (2D) and three-dimensional (3D) regions of interest (ROI) were integral to the analytical framework, yielding tens of thousands of quantitative imaging biomarkers indicative of texture, shape, and intensity distribution.
Through a methodical feature selection process, the researchers distilled these extensive datasets down to the most predictive radiomics signatures: 28 key features from 2D ROIs and 15 from 3D ROIs. Logistic regression classifiers were then employed to build radiomics signatures, with the 3D multiparametric model—encompassing combined T1WI, T2WI, and CE-T1 imaging—demonstrating superior predictive performance. Quantitatively, this 3D multi-sequence radiomics signature achieved an area under the receiver operating characteristic curve (AUC) of approximately 0.79 in both training and internal validation data, reflecting a high degree of accuracy.
Recognizing that radiomics alone might not capture the full clinical complexity, the research further integrated significant clinical risk factors—identified through univariate and multivariate analyses—with radiomic features to form comprehensive clinical-radiomics models. Notably, models incorporating both 2D and 3D ROI features alongside clinical data outperformed others, achieving AUCs nearing 0.89 during training and maintaining robust validation performance with AUCs above 0.81.
The construction of a nomogram based on these clinical-radiomics models offers a practical and intuitive tool for clinicians to apply preoperative consistency predictions in real-world settings. Especially valuable is the model’s validation on external, multicenter datasets, which underscores its generalizability and potential for widespread clinical deployment across diverse patient populations and imaging platforms.
The implications of this research extend beyond immediate surgical planning. Preoperative knowledge of tumor consistency could influence the choice of surgical approach—whether endoscopic or microscopic transsphenoidal surgery—anticipate the need for adjunctive treatments, or even guide biopsy decisions. Soft tumors typically afford easier resection and reduced operative time, whereas hard tumors may necessitate more complex maneuvers, underscoring the prognostic utility of this imaging-based predictive capability.
From a technical standpoint, the implementation of multiparametric MRI sequences ensures comprehensive tissue characterization by harnessing differences in tumor cellularity, vascularity, and necrotic components. Radiomics quantitatively captures these features, transcending the subjective interpretations of conventional radiology through sophisticated algorithms capable of pattern recognition and statistical modeling.
This effort exemplifies the growing fusion of artificial intelligence, medical imaging, and clinical oncology, where data-rich radiomic analyses complement traditional diagnostic pathways. The use of logistic regression classifiers, alongside rigorous feature selection and validation protocols, provides methodological robustness that paves the way towards clinical translation and integration into decision support systems.
Importantly, the study highlights the distinct predictive efficiencies between 2D and 3D ROI-based radiomics models, advocating for a combined approach to leverage the strengths of both dimensional analyses. The 3D models, for instance, may better capture the volumetric heterogeneity and spatial distribution of tumor texture, while 2D features can provide finer resolution details within specific slices.
Given the increasing prevalence of PitNETs and their clinical challenge, particularly due to variable tumor textures influencing surgical morbidity, these findings herald a new era of precision medicine in pituitary surgery. Surgeons equipped with preoperative knowledge of tumor consistency may optimize operative tactics, potentially reducing complications such as cerebrospinal fluid leaks, hemorrhage, or incomplete resections.
Future research directions suggested by these investigators include prospective validation studies, expansion into other tumor types exhibiting consistency-related surgical challenges, and integration with other omics data streams such as genomics and proteomics to enhance predictive modeling further.
In conclusion, this multicenter study robustly demonstrates that multiparametric MRI radiomics is a powerful, non-invasive modality for the preoperative prediction of PitNET consistency. The combination of advanced imaging techniques, comprehensive feature extraction, and sophisticated statistical modeling underpins a clinical tool with significant potential to improve the management paradigms of pituitary neuroendocrine tumors.
Article Title: Preoperative prediction of pituitary neuroendocrine tumor consistency based on multiparametric MRI radiomics: a multicenter study
Article References: Yang, Q., Wang, Y., Wu, J. et al. Preoperative prediction of pituitary neuroendocrine tumor consistency based on multiparametric MRI radiomics: a multicenter study. BMC Cancer 25, 1501 (2025). https://doi.org/10.1186/s12885-025-14799-1
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14799-1