In a groundbreaking study conducted by the Medical University of Vienna, researchers have uncovered compelling insights into the impact of socioeconomic factors on neurological outcomes following out-of-hospital cardiac arrest (OHCA). The comprehensive analysis, presented at the European Emergency Medicine Congress, reveals that, intriguingly, neurological recovery trajectories post-cardiac arrest at home do not significantly differ across income brackets despite underlying disparities in pre-hospital interventions such as bystander cardiopulmonary resuscitation (CPR).
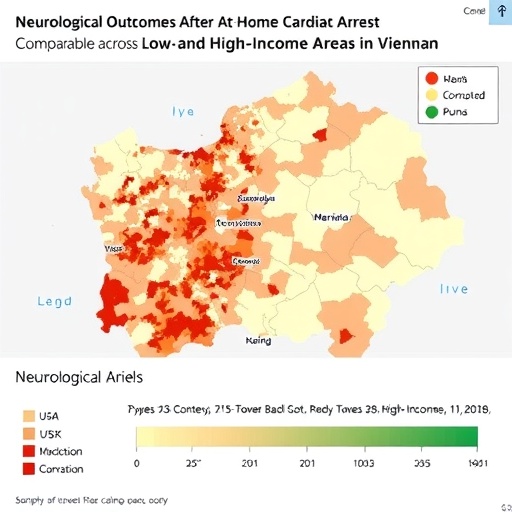
Led by Drs. Jürgen Grafeneder and Christoph Schriefl, the investigative team meticulously examined data from 676 adult patients treated for OHCA in Vienna’s Department of Emergency Medicine between January 2020 and December 2022. The study integrated clinical registry information with socioeconomic indicators derived from patients’ residential addresses, mapping these to electoral districts and corresponding average household incomes using Austria’s National Statistical System. This innovative geosocial linkage provided a nuanced framework to explore income-related disparities in emergency cardiac care outcomes.
A focal point of this research was the assessment of patients’ neurological status at multiple post-arrest intervals—one, six, and twelve months—allowing for a longitudinal understanding of cognitive recovery and functional brain integrity. Neurological outcomes were quantified using established clinical metrics evaluating brain damage severity and cognitive functioning, offering a clinically meaningful lens through which socioeconomic influences could be scrutinized amid confounding variables such as patient comorbidities and pre-hospital therapeutic interventions.
Despite prior assumptions that socioeconomic status would significantly influence survival and neurological recovery, the findings defied expectations. The researchers found no statistically significant association between income quartiles and neurological outcomes among patients who survived to hospital admission. This critical insight suggests that once patients overcome the initial life-threatening phase of cardiac arrest and are successfully enrolled in tertiary care, socioeconomic disparities exert a minimal effect on brain recovery.
Yet, an important caveat emerged regarding the prevalence of bystander CPR before emergency responders arrived. The data suggested a trend where individuals residing in Vienna’s lower income quartiles received bystander CPR less frequently (64%) compared to those in higher income areas (78%), although this trend lacked statistical significance. Experts highlight that this observed disparity, while not definitive, may signal systemic inequities in community readiness and public health education aimed at CPR training across socioeconomic strata.
Medical student Hannah Voith, who presented the findings, emphasized the crucial interplay between social determinants and emergency responsiveness. She noted that enhancing public health strategies to improve basic life support knowledge could dramatically influence survival rates and neurological outcomes if implemented widely and equitably. The study underlines the latent potential of targeted interventions to amplify bystander CPR rates and thereby mitigate survival disparities rooted in socioeconomic divides.
Another significant aspect of the study is the recognition of inherent selection biases linked to the study cohort. Since only patients admitted to the hospital were included, the data potentially exclude those who died pre-hospital due to absent or inadequate bystander CPR. This attrition effect likely filters out the most severe impact of socioeconomic barriers on cardiac arrest survival, meaning real-world disparities could be even starker than reported.
Professor Felix Lorang, an independent emergency medicine expert from Germany, highlighted the broader implications of the findings. He pointed to the critical importance of early CPR administration post-arrest and acknowledged the need to investigate further the observed trend of lower bystander CPR rates in socioeconomically disadvantaged neighborhoods. Advocacy for widespread CPR training and public awareness campaigns remains paramount to advancing emergency cardiac care on a global scale.
Interestingly, the Vienna study stands as the first in Austria to synergize granular registry data with geospatial economic analysis to elucidate this delicate relationship between social determinants and neurological recovery. The multi-dimensional approach not only enriches epidemiological understanding but also provides policymakers with actionable intelligence to develop precision interventions grounded in regional social vulnerabilities.
Nonetheless, the researchers acknowledge limitations, including the observational nature of the study and reliance on aggregated socioeconomic data rather than individual-level income metrics. Additionally, infrastructural variables such as proximity to specialized facilities like Vienna General Hospital might have confounded outcomes but were beyond the scope of the dataset. Future research endeavors aim to incorporate these factors alongside longitudinal assessments extending to patients receiving advanced therapies like extracorporeal cardiopulmonary resuscitation (ECPR).
Looking forward, the team plans to broaden the geographic scope of their investigations to include other Austrian urban centers like Graz to validate findings and contextualize Vienna’s unique emergency services infrastructure. Expanding the epidemiological framework to capture community-level bystander CPR trends citywide and analyzing long-term neurological outcomes will further refine understanding of socioeconomic influences on cardiac arrest prognosis.
This seminal work underscores the complex interdependence of public health systems, community engagement, and clinical outcomes in emergency medicine. It calls for reinforced investment in accessible first aid education programs and inclusive health policies to uplift survival chances and quality of life after out-of-hospital cardiac arrest, especially within underserved populations.
In sum, while socioeconomic status does not appear to modulate neurological recovery among hospitalized cardiac arrest survivors in Vienna, the potential disparities in immediate, life-saving care before hospital arrival warrant rigorous attention. Bridging these gaps through targeted public health initiatives could unleash substantive benefits in survival rates and functional recovery, illuminating a pathway toward more equitable emergency care ecosystems.
Subject of Research: People
Article Title: The impact of socioeconomic factors on the outcome in adult out-of-hospital cardiac arrest patients – a retrospective data analysis
News Publication Date: 1-Oct-2025
Image Credits: Hannah Voith
Keywords: Cardiac arrest, Neurological disorders, Amnesia, Cognitive disorders, Cardiology, Human heart, Medical treatments, Resuscitation, Health care, Emergency medicine, Health care delivery
Tags: adult patient outcomes in emergency medicinebystander CPR impact on survival ratescardiac arrest recovery in low-income areasclinical metrics for brain damage evaluationemergency medicine research findingsgeosocial analysis in healthcareincome-related disparities in cardiac carelongitudinal assessment of cognitive recoveryneurological outcomes after cardiac arrestneurological recovery trajectories in high-income settingsout-of-hospital cardiac arrest study Viennasocioeconomic factors in emergency medicine