In a groundbreaking study published in BMC Cancer, researchers have unveiled a novel link between the nasopharyngeal microbiota and the onset of post-radiation nasopharyngeal necrosis (PRNN) in patients undergoing re-irradiation for recurrent nasopharyngeal carcinoma (NPC). This discovery sheds light on an urgently needed predictive tool for a severe and often debilitating complication, offering hope for early intervention and improved patient outcomes.
Nasopharyngeal carcinoma, a malignancy originating in the upper part of the throat behind the nose, often necessitates radiation therapy as a frontline treatment. However, disease recurrence is common, and re-irradiation, while potentially lifesaving, carries significant risks. Among these, PRNN stands out as a devastating complication marked by tissue death following repeated radiation exposure, leading to severe morbidity and diminished quality of life. Understanding and predicting which patients are most vulnerable to PRNN has remained elusive, frustrating oncologists and clinicians worldwide.
The research team conducted a comprehensive retrospective analysis of 113 patients treated at the Sun Yat-sen University Cancer Center between January 2020 and November 2022. All individuals had recurrent NPC and underwent re-irradiation. They meticulously categorized patients into two groups—those who developed nasopharyngeal necrosis post-treatment and those who did not. Prior to re-irradiation, nasopharyngeal biopsy tissues were collected to characterize the microbiota landscape through 16S ribosomal RNA sequencing, an advanced technology that allows precise profiling of microbial communities.
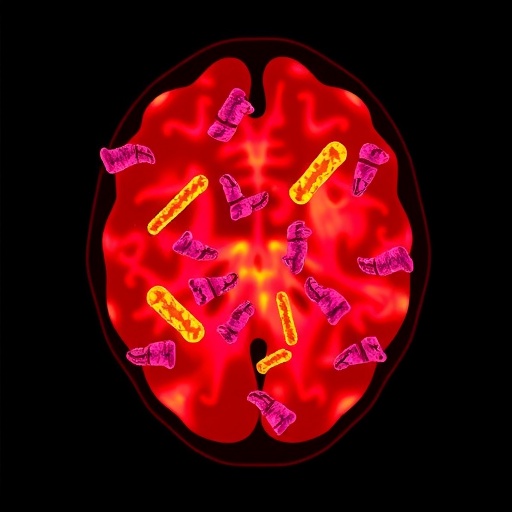
Initial findings confirmed that the dominant bacterial phyla within the nasopharynx comprised Proteobacteria and Firmicutes across all patients, reaffirming previous knowledge about the microbiome’s role in this anatomical niche. Intriguingly, the group that went on to develop necrosis exhibited significantly higher alpha diversity, indicating a more complex and varied microbial ecosystem compared to their counterparts. This elevated diversity might reflect an underlying dysbiosis—an imbalance in microbial communities—that potentially predisposes tissue to radiation-induced damage.
Furthermore, the study identified pronounced differences in beta diversity, suggesting that the microbial composition between necrosis and non-necrosis groups diverged considerably. This distinct microbial fingerprint lays the foundation for microbiota-based biomarkers that could forecast PRNN risk with remarkable accuracy. The researchers leveraged this insight to develop a sophisticated predictive model combining clinical variables, notably gross tumor volume (GTV), with microbiome signatures.
Utilizing a random forest classifier—a machine learning algorithm adept at handling complex data—they trained and tested the model on patient datasets. Performance metrics were striking: an area under the curve (AUC) of 87.9% in the training phase and 86.9% in validation sets demonstrated that the integrated model robustly discriminates patients at risk of necrosis. These predictive capabilities promise to revolutionize clinical decision-making, allowing tailored treatment regimens that mitigate life-threatening complications.
The implications of these findings are profound. Current strategies to manage recurrent NPC and its complications rely heavily on imaging and clinical judgment, which often occur too late to prevent necrosis. With microbiota profiling entering the diagnostic arena, clinicians could identify vulnerable patients before re-irradiation, enabling preemptive interventions such as microbiome modulation, targeted antibiotics, or dose adjustments.
This study also opens avenues for exploring the causal mechanisms linking microbial diversity to tissue necrosis. The nasopharyngeal microbiota’s role in modulating inflammation, immune responses, and epithelial integrity likely influences radiation tolerance. Dysbiotic microbial communities may exacerbate oxidative stress or impair mucosal healing, triggering necrotic pathways. Deciphering these interactions at a molecular level could unveil novel therapeutic targets to safeguard normal tissue during aggressive oncologic therapies.
Moreover, the methodology employed demonstrates the power of integrating omics data with clinical parameters through artificial intelligence. As personalized medicine advances, the ability to capture and interpret complex biological and clinical datasets will become indispensable. This study exemplifies how such integrative approaches can translate into tangible clinical benefits in oncology.
While promising, the research is retrospective and warrants prospective validation across diverse populations and clinical settings. The heterogeneity of the nasopharyngeal microbiota across ethnicities, geographies, and environmental exposures must be accounted for. Additionally, the dynamic changes in microbiota during and post-radiation therapy remain to be elucidated, which could refine prognostic models further.
In conclusion, the identification of nasopharyngeal microbial diversity as a predictive biomarker for PRNN marks a significant advancement in the management of recurrent NPC. By marrying microbiology with machine learning, the study offers a potent tool to foresee and forestall a devastating treatment complication. This integrative approach exemplifies the future of cancer care, where precision diagnostics inform bespoke therapeutic strategies, improving survival and quality of life for patients facing formidable diseases.
As oncologists, microbiologists, and data scientists continue to unravel the nexus between the human microbiome and cancer therapy outcomes, studies such as this reinforce the message that microbes are not mere bystanders but active participants in human health and disease. Harnessing this knowledge promises to transform cancer management, highlighting a new frontier in personalized oncology.
Subject of Research: The predictive value of nasopharyngeal microbiota for post-radiation necrosis following re-irradiation in recurrent nasopharyngeal carcinoma.
Article Title: Predictive value of nasopharyngeal microbiota for necrosis after re-irradiation in recurrent nasopharyngeal carcinoma.
Article References: Wen, K., Huang, ZR., Liu, YL. et al. Predictive value of nasopharyngeal microbiota for necrosis after re-irradiation in recurrent nasopharyngeal carcinoma. BMC Cancer 25, 1436 (2025). https://doi.org/10.1186/s12885-025-14842-1
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14842-1
Tags: innovative cancer research findingsmicrobiota and cancer treatmentnasopharyngeal biopsy analysisnasopharyngeal microbiotanecrosis after radiation therapypatient outcomes in NPCpost-radiation necrosis predictionpredictive tools in oncologyre-irradiation complicationsrecurrent nasopharyngeal carcinoma treatmentsevere morbidity in cancer patientsSun Yat-sen University Cancer Center study