In the relentless fight against one of the deadliest brain cancers, glioblastoma, a groundbreaking study published in Nature Communications is reshaping the diagnostic landscape. Glioblastoma, known for its aggressive nature and poor prognosis, has long posed a significant challenge for radiologists and oncologists alike, particularly when it comes to accurately distinguishing it from other brain lesions that mimic its appearance on imaging studies. The new research, conducted by Zhao et al., introduces a sophisticated ensemble of foundation models equipped with an uncertainty-aware mechanism—an innovative advancement that is poised to revolutionize diagnostic precision and patient outcomes in neuro-oncology.
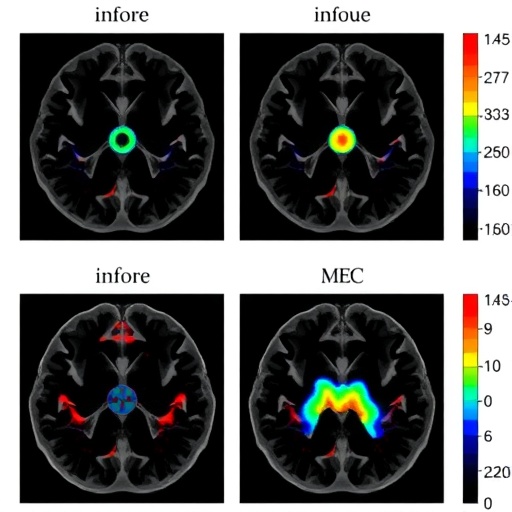
This new methodology integrates multiple large-scale artificial intelligence models, commonly referred to as foundation models, to analyze complex imaging data. What sets this system apart is its unique ability to account for uncertainty in predictions, a critical factor when making decisions that impact treatment strategies for patients with suspected glioblastoma. By assessing not just the data itself but the confidence in each prediction, the model provides a nuanced diagnostic output that enhances the reliability of the differentiation process. This subtle but transformative shift addresses a longstanding gap in radiological assessments, where ambiguous cases often lead to diagnostic uncertainty and, consequently, suboptimal clinical decision-making.
The foundation models employed are tailored neural networks trained on vast amounts of diverse medical imaging data, enabling them to capture intricate patterns beyond human visual perception. Their capability to generalize across various types of brain lesions is complemented by the ensemble framework, which synergizes the strengths of individual models while mitigating individual weaknesses. This ensures that the combined output is robust against errors that might arise from variations in imaging quality, patient demographics, or tumor heterogeneity. Crucially, the incorporation of uncertainty quantification safeguards against overconfident yet incorrect predictions, offering clinicians a transparent risk assessment alongside diagnostic suggestions.
Glioblastomas are notoriously challenging to distinguish from other gliomas and non-neoplastic lesions such as abscesses, metastases, or demyelinating diseases, all of which can exhibit overlapping radiologic features. Traditional imaging modalities often rely heavily on subjective interpretation, influenced by radiologist experience and available clinical information. This new ensemble approach shifts the paradigm towards objective, data-driven decision-making. The precision of this AI-driven diagnostic tool lies not only in its ability to correctly identify glioblastomas but also in its proficiency at flagging cases where the confidence is low, prompting further investigation rather than premature therapeutic interventions.
The study’s methodology harnessed annotated brain MRI datasets obtained from multiple institutions, encompassing a heterogeneous mix of glioblastoma presentations and their mimics. The models were trained, validated, and tested through rigorous protocols that ensured generalizability and minimized overfitting. Performance metrics documented in the paper demonstrate a marked improvement over traditional single-model AI approaches and conventional radiological assessments. Notably, the uncertainty-aware ensemble achieved higher sensitivity and specificity rates, with statistically significant reductions in false-positive and false-negative rates, which are critical factors in clinical scenarios where the therapeutic window is narrow and treatment-related risks are profound.
Another crucial aspect of this research is its potential incorporation into clinical workflows. Unlike many AI studies that remain confined to theoretical or preclinical phases, this work emphasizes the translational aspect, providing a clear roadmap for integration into hospital information systems and PACS (Picture Archiving and Communication Systems). The real-time or near-real-time capability of the ensemble model enables rapid second opinions, potentially reducing diagnostic turnaround times and enhancing multidisciplinary team discussions. Moreover, the uncertainty metrics serve as a decision support tool that can improve the confidence of less experienced radiologists or serve as a safeguard for well-trained specialists facing complex cases.
The inherent complexity of glioblastoma diagnosis is further compounded by the tumor’s heterogeneity at molecular and histopathological levels. By focusing on imaging biomarkers and machine learning interpretations informed by diverse data inputs, the ensemble approach bridges the gap between radiologic appearance and underlying pathology. This synergy opens new avenues for personalized medicine, where treatment plans can be more accurately tailored to the individual patient’s tumor biology. Additionally, early and accurate diagnosis facilitated by this AI tool can expedite timely surgical intervention, targeted radiotherapy, and chemotherapy, all of which are pivotal for extending survival and improving quality of life.
Importantly, the inclusion of uncertainty quantification aligns with a broader movement in AI toward responsible and ethical deployment. Overreliance on AI systems without understanding their limitations poses risks in critical care settings. By explicitly modeling and communicating the confidence of diagnostic outputs, this framework promotes transparency and accountability. This novel mechanism allows clinicians to view AI as an adjunct rather than a replacement, fostering trust and collaboration between human experts and machine intelligence. Such partnerships are vital in fields like neuro-oncology, where stakes are high and diagnostic errors can have devastating consequences.
The impact of this research extends beyond glioblastoma. The ensemble and uncertainty-aware modeling paradigm can be adapted to many other medical domains fraught with diagnostic ambiguity, such as pulmonary nodules, pancreatic lesions, and musculoskeletal tumors. The modular nature of foundation models and their capacity to learn from multimodal data—including imaging, genomics, and clinical histories—mean that this approach could become a cornerstone of comprehensive diagnostic AI ecosystems in the near future. As healthcare systems increasingly adopt digital technologies, the ability to harness large-scale, interpretable AI with uncertainty measures will be essential for scaling expert-level diagnostics across diverse patient populations and healthcare settings.
In essence, Zhao et al.’s study represents a crucial step toward closing the diagnostic gap in neuro-oncology using cutting-edge AI technologies. Their work highlights how advanced machine learning frameworks, designed with clinical realities and uncertainties in mind, can provide actionable intelligence for complex disease differentiation. This progress is not merely academic; it has profound implications for patient care pathways, resource allocation, and ultimately, survival rates. As glioblastoma continues to pose a significant challenge worldwide, innovations like this bring hope for improved diagnostic confidence, earlier interventions, and more personalized therapies that can change the natural history of this lethal disease.
The research also underscores the importance of collaboration between computational scientists, radiologists, oncologists, and data engineers. Achieving such sophisticated AI models requires not only technical expertise but also domain knowledge that informs model architecture, data curation, and clinical validation. The interdisciplinary nature of this work exemplifies how modern medical breakthroughs are increasingly reliant on joining forces across specialties. Such teamwork ensures that AI tools are not developed in isolation but are tightly aligned with clinical workflows and patient outcomes, thereby maximizing their utility and adoption in real-world settings.
Moreover, this model’s ability to manage diagnostic uncertainty is a significant advancement beyond traditional AI diagnostics, which often offer binary or overly simplistic outputs. By incorporating a probabilistic perspective, Zhao et al.’s ensemble encourages a reinterpretation of AI outputs as part of a broader clinical context—one that integrates human judgment, additional testing, and patient preferences. This nuanced approach may ultimately reduce the incidence of premature or inappropriate treatments driven by overconfident machine recommendations, safeguarding patient safety and enhancing personalized care strategies.
Future directions prompted by this work are numerous. Additional studies are expected to explore the integration of advanced multimodal inputs such as PET imaging, functional MRI, and histopathological digitized slides into the ensemble framework, potentially improving diagnostic granularity even further. Longitudinal analyses may allow AI to not only differentiate glioblastoma at baseline but also predict progression, recurrence, or treatment response. Such prognostic tools could transform patient monitoring and adaptive therapy strategies, paving the way for dynamic, AI-augmented clinical decision-making tailored to individual patient trajectories.
In conclusion, the introduction of an uncertainty-aware ensemble of foundation models signifies a paradigm shift in the way glioblastoma and its mimicking lesions can be differentiated using AI. By combining state-of-the-art machine learning methodologies with a transparent confidence framework, Zhao and colleagues have opened the door to more precise, reliable, and clinically meaningful brain tumor diagnostics. Their contribution is a testament to the power of AI to augment, not replace, human expertise and represents a beacon of hope in the ongoing battle against one of the most devastating cancers. As this technology proliferates and matures, patients, clinicians, and researchers alike stand to benefit from the enhanced clarity and nuance it brings to the urgent task of neuro-oncological diagnosis.
Subject of Research: Differentiation of glioblastoma from its mimicking lesions using an uncertainty-aware ensemble of foundation AI models.
Article Title: Uncertainty-aware ensemble of foundation models differentiates glioblastoma from its mimics.
Article References:
Zhao, J., Lin, SY., Attias, R. et al. Uncertainty-aware ensemble of foundation models differentiates glioblastoma from its mimics. Nat Commun 16, 8341 (2025). https://doi.org/10.1038/s41467-025-64249-6
Image Credits: AI Generated
Tags: artificial intelligence in neuro-oncologyconfidence in medical predictionsdistinguishing brain lesionsenhancing diagnostic precisionglioblastoma diagnosisimaging studies in glioblastomainnovative cancer researchNature Communications study on glioblastomapredictive modeling in cancerradiological assessments for glioblastomatreatment strategies for brain canceruncertainty-aware models