In a groundbreaking advancement at the intersection of artificial intelligence and neuro-oncology, a Harvard Medical School–led team has introduced a novel AI tool capable of discriminating between two visually similar yet biologically distinct brain tumors with unprecedented accuracy. This innovation holds transformative potential for surgical oncology by providing real-time diagnostic insights directly within the operating theater, enabling critical intraoperative decision-making.
The AI system, named PICTURE (Pathology Image Characterization Tool with Uncertainty-aware Rapid Evaluations), addresses one of neuro-oncology’s most pressing diagnostic challenges: differentiating glioblastoma — the brain’s most aggressive and prevalent tumor — from primary central nervous system lymphoma (PCNSL), a rarer malignancy originating from immune cells. Both tumors often mimic each other’s histological appearance under the microscope, leading to frequent misdiagnoses that can drastically impact treatment choices and patient outcomes.
Glioblastomas, deriving from neuroglial cells, require extensive surgical excision followed by targeted therapies. In contrast, PCNSL, which are lymphoid in origin, typically respond better to radiation and chemotherapy, and surgery tends to offer minimal benefit. This divergence in treatment paradigms underscores the critical need for precise, immediate tumor identification during brain surgery to tailor interventions appropriately and avoid unnecessary tissue removal or treatment delays.
Standard intraoperative evaluation involves a frozen section analysis of resected tissue samples, which, while rapid, introduces artifacts that complicate cellular morphology interpretation. This can result in diagnostic inconsistencies; studies have noted that approximately 5% of initial intraoperative tumor diagnoses are revised upon subsequent detailed pathological examination. The PICTURE AI tool emerges as a solution to minimize such discrepancies by supplementing the expertise of surgeons and pathologists with advanced computational assessment that operates effectively even on these distorted frozen tissue sections.
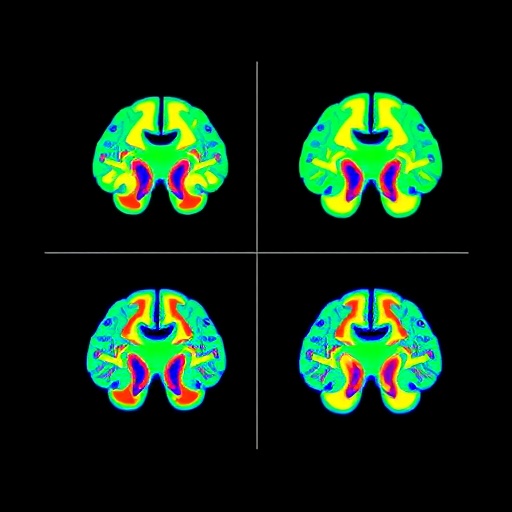
PICTURE’s architecture integrates an ensemble of foundational AI models, collectively trained and validated on an extensive dataset comprising over 2,100 brain pathology slides, sourced globally and encompassing diverse specimen preparation methods. This robust data foundation enabled the tool to learn subtle morphological markers such as cell density variations, nuclear atypia, necrosis patterns, and cellular shape irregularities that distinguish glioblastomas from PCNSL with remarkable precision.
What sets PICTURE apart from previous AI endeavors in the domain is not only its superior classification accuracy—exceeding 98% across multiple international validation cohorts—but also its embedded uncertainty-detection mechanism. This feature empowers the AI to recognize when it encounters tumor presentations outside its trained repertoire, effectively flagging ambiguous cases for immediate human expert review rather than forcing an erroneous binary classification. Such an uncertainty-aware design is vital, given that over 100 brain tumor subtypes exist, many of which are rare and bear overlapping characteristics.
Performance evaluations conducted across five hospitals spanning four countries demonstrated consistent outperformance of PICTURE relative to veteran neuropathologists and existing AI diagnostic frameworks. In clinical scenarios marked by expert disagreement, which historically saw misdiagnoses in up to 38% of complex cases, PICTURE reliably provided accurate tumor identity, bolstering diagnostic confidence and potentially improving patient care pathways.
The real-world application of PICTURE in operating rooms promises to revolutionize neurosurgical oncology workflows by offering immediate, data-driven insights during tumor resections. This capability supports timely surgical decisions, such as the extent of tissue removal or the necessity of adjuvant treatments, that can influence both short-term operative success and long-term neurological function preservation.
Beyond intraoperative utility, the tool holds significant potential to democratize specialized neuropathology assessment, a field suffering from global shortages of expert diagnosticians and uneven geographic distribution. By providing universally accessible AI assistance, PICTURE could elevate standards of care in resource-constrained settings and serve as an educational platform to train budding pathologists on the nuanced morphological distinctions among challenging brain tumors.
Though initially focused on glioblastoma and PCNSL differentiation, future iterations of the AI system might integrate genetic, molecular, and genomic data layers to refine tumor subclassification, prognostic predictions, and personalized therapy recommendations. The researchers acknowledge that most training samples originated from patients of white ethnicity, highlighting the need for further validation across ethnically diverse populations to ensure broad applicability and fairness.
Support for this innovative work derived from a confluence of public and private sources, including grants from the National Institutes of Health, the American Cancer Society, and pioneering awards from Google Research and Harvard Medical School. Transparency regarding intellectual property and potential conflicts was also maintained, underscoring the study’s academic rigor and commitment to open scientific collaboration.
PICTURE’s inception marks a promising step toward harnessing AI not just as a diagnostic adjunct but as an integral partner in clinical care, capable of navigating the complex histopathological landscape of brain tumors with finesse and reliability. Ultimately, such technologies may usher in an era where computational precision complements human expertise to dramatically improve survival and quality of life for patients battling formidable brain cancers.
Subject of Research: AI-based diagnostic differentiation of glioblastoma and primary central nervous system lymphoma during brain surgery
Article Title: Uncertainty-aware ensemble of foundation models differentiates glioblastoma from its mimics
News Publication Date: September 29, 2025
Web References: https://www.nature.com/articles/s41467-025-64249-6
References: DOI: 10.1038/s41467-025-64249-6
Keywords: Artificial intelligence, Glioblastoma cells, Cancer, Brain tumors
Tags: advanced imaging techniques in medicineAI applications in surgeryAI in neuro-oncologybrain surgery decision-makingglioblastoma vs primary central nervous system lymphomahistological tumor identificationintraoperative diagnostic toolspatient outcomes in brain cancer treatmentPICTURE AI toolreal-time brain tumor differentiationsurgical oncology innovationstumor misdiagnosis consequences