A groundbreaking study recently published in Acta Pharmaceutica Sinica B has shed new light on the molecular mechanisms underlying cerebral ischemia–reperfusion (I/R) injury, a devastating consequence of stroke. Researchers have identified the protein arginine methyltransferase PRMT1 as a crucial regulator that ameliorates brain injury by directly suppressing the activation of receptor-interacting protein kinase 1 (RIPK1), a key mediator of cell death pathways. This revelation opens promising avenues for novel therapeutic strategies aimed at reducing neuronal loss and improving outcomes following ischemic stroke.
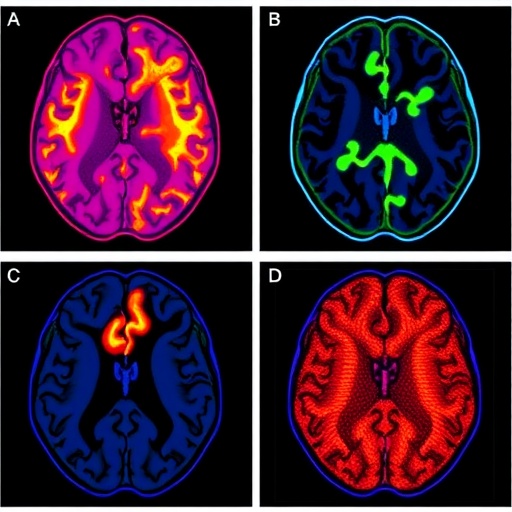
Cerebral ischemia–reperfusion injury occurs when blood supply to the brain is temporarily interrupted and then restored, paradoxically leading to further neuronal damage. One of the pathological mechanisms responsible for such injury is programmed cell death. RIPK1, a serine/threonine kinase, has emerged as a master regulator orchestrating necroptosis and apoptosis during I/R events. Necroptosis is a form of regulated necrosis characterized by cellular swelling and membrane rupture, while apoptosis is a form of programmed cell death involving cellular shrinkage and DNA fragmentation. Both pathways contribute significantly to ischemic brain injury.
Despite the pivotal role of RIPK1 in mediating cell death, the precise regulatory checkpoints governing its activation in the context of cerebral I/R injury have remained unknown until now. The investigative team, led by scientists including Tengfei Liu, Gan Huang, and colleagues, explored the role of PRMT1, a protein that methylates arginine residues on target proteins, thereby modulating their function. Their findings reveal that PRMT1 expression is markedly downregulated following cerebral I/R injury, setting off a cascade that culminates in the activation of RIPK1.
Mechanistically, the study demonstrates that PRMT1 physically interacts with RIPK1 and catalyzes asymmetric dimethylation of its arginine residues. This post-translational modification effectively inhibits RIPK1 homodimerization—a prerequisite for its kinase activation. Inhibition of homodimerization leads to the suppression of RIPK1’s kinase activity, which in turn prevents the initiation of downstream cell death pathways such as necroptosis and apoptosis. This regulatory axis provides a novel molecular safeguard against excessive neuronal death.
To validate the functional significance of this interaction, the researchers employed pharmacological inhibitors and genetic ablation techniques to reduce PRMT1 activity in experimental models of cerebral I/R injury. Under these conditions, they observed exacerbated brain damage characterized by increased RIPK1 activation and enhanced necroptotic and apoptotic cell death. Conversely, overexpression of PRMT1 conferred neuroprotection by attenuating RIPK1 activity and reducing neuronal loss.
This dual approach highlights the potential of PRMT1 modulation as a therapeutic strategy. The attenuation of RIPK1-mediated necroptosis and apoptosis through restoring or augmenting PRMT1 activity could serve as a novel intervention point to mitigate ischemic stroke outcomes. The study further reinforces the complexity of post-translational modifications in fine-tuning kinase signaling and cell fate decisions under pathological conditions.
The study also advances our understanding of the crosstalk between methylation and phosphorylation events in regulating intracellular signaling during brain injury. Arginine methylation carried out by enzymes such as PRMT1 represents a reversible and dynamic modification that can modulate protein-protein interactions and enzymatic activities. In the context of cerebral I/R injury, PRMT1-dependent methylation of RIPK1 acts as an inhibitory checkpoint that restrains kinase-driven cell death.
Necroptosis, driven by RIPK1 kinase activity, involves the recruitment and phosphorylation of mixed lineage kinase domain-like pseudokinase (MLKL), leading to plasma membrane permeabilization and necrotic cell death. Apoptosis, on the other hand, is characterized by caspase activation and cellular dismantling. RIPK1 is uniquely positioned as a signaling hub that determines cell fate by balancing these pathways. The identification of PRMT1 as a negative regulator of RIPK1 highlights a sophisticated molecular switch controlling neuronal survival.
Given the high global burden of ischemic stroke and the limited therapeutic options currently available, the discovery of PRMT1’s protective role against cerebral I/R injury carries significant clinical implications. Strategies aimed at enhancing PRMT1 activity or mimicking its methylation effect on RIPK1 may limit the extent of neuronal damage and improve neurological recovery in stroke patients.
Moreover, the study underscores the value of targeting post-translational modifications as a pharmacological approach. Unlike irreversible genetic alterations, modulating enzyme activities such as PRMT1 offers potential reversibility and temporal control, making it an attractive route for drug development. Future research will be required to identify selective activators or stabilizers of PRMT1 that can be translated into clinical applications.
The authors also call attention to the necessity for deeper mechanistic studies to delineate whether PRMT1 exerts additional neuroprotective effects beyond RIPK1 methylation. It is plausible that PRMT1 may regulate other signaling targets or pathways involved in inflammation, oxidative stress, or cellular metabolism during cerebral ischemia–reperfusion injury. Comprehensive proteomic and interactome analyses may uncover such layers of regulation.
In conclusion, the elucidation of PRMT1 as a key modulator that suppresses RIPK1-mediated necroptosis and apoptosis represents a landmark advancement in stroke biology. This work not only enriches our molecular understanding of neuronal cell death regulation but also establishes PRMT1 as a promising target for the development of therapies aimed at protecting the brain from ischemic injury. As research progresses, it will be critical to translate these insights into pharmacological strategies that can effectively reduce morbidity and mortality associated with ischemic stroke worldwide.
Subject of Research: Regulation of RIPK1 kinase activity and neuronal cell death mechanisms in cerebral ischemia–reperfusion injury
Article Title: The protein arginine methyltransferase PRMT1 ameliorates cerebral ischemia–reperfusion injury by suppressing RIPK1-mediated necroptosis and apoptosis
News Publication Date: 2025
Web References:
Acta Pharmaceutica Sinica B: https://www.sciencedirect.com/journal/acta-pharmaceutica-sinica-b
DOI: http://dx.doi.org/10.1016/j.apsb.2025.06.005
References:
Liu, T., Huang, G., Guo, X., Ji, Q., Yu, L., Zong, R., Li, Y., Song, X., Fu, Q., Xue, Q., Zheng, Y., Zeng, F., Sun, R., Chen, L., Gao, C., Liu, H. (2025). The protein arginine methyltransferase PRMT1 ameliorates cerebral ischemia–reperfusion injury by suppressing RIPK1-mediated necroptosis and apoptosis. Acta Pharmaceutica Sinica B, 15(8), 4014-4029.
Keywords: PRMT1, Cerebral ischemia–reperfusion injury, RIPK1, Arginine methylation, Necroptosis, Apoptosis, Phosphorylation, MLKL
Tags: cerebral ischemia-reperfusion injury mechanismsischemic stroke treatment advancementsmolecular mechanisms of stroke damagenecroptosis and apoptosis in neuronal damageneuronal loss after ischemic strokeneuroprotection in cerebral ischemiaPRMT1 protein role in brain ischemiaprogrammed cell death in ischemic brain injuryprotein arginine methyltransferase researchregulation of RIPK1 activationRIPK1-mediated cell death pathwaystherapeutic strategies for stroke recovery