In recent years, the field of endocrinology has witnessed significant advancements, particularly in the understanding of polycystic ovary syndrome (PCOS), a common endocrine disorder affecting women of reproductive age. One of the critical markers in assessing ovarian function and health in women diagnosed with PCOS is Anti-Müllerian Hormone (AMH). Recent research conducted by Wang et al. provides invaluable insights into developing age-specific AMH screening cutoffs tailored for Chinese women suffering from PCOS. This retrospective study utilizes propensity score matching analysis, a robust statistical technique that attempts to reduce bias in estimation by equating groups based on certain characteristics.
The investigation begins with a thorough understanding of PCOS, a multifaceted disorder characterized by hormonal imbalance, hyperandrogenism, and often, insulin resistance. Women with PCOS frequently experience complications that can impact their reproductive health as well as metabolic function. With this context established, the study sets out to delve deeper into the utility of AMH as a biomarker, especially across different age groups within the population of Chinese women diagnosed with this condition.
AMH is a glycoprotein hormone produced by the ovarian follicles. Its levels are indicative of the ovarian reserve, which refers to the number of viable oocytes (egg cells) remaining in a woman’s ovaries. The correlation between AMH levels and age has been a topic of interest, especially since AMH levels tend to decrease as women grow older. The findings of Wang et al. aim to elevate our understanding of these dynamics specific to the demographic of Chinese women with PCOS, who may exhibit different AMH profiles compared to their counterparts across different regions and ethnicities.
.adsslot_Jbpmw43OSr{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_Jbpmw43OSr{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_Jbpmw43OSr{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
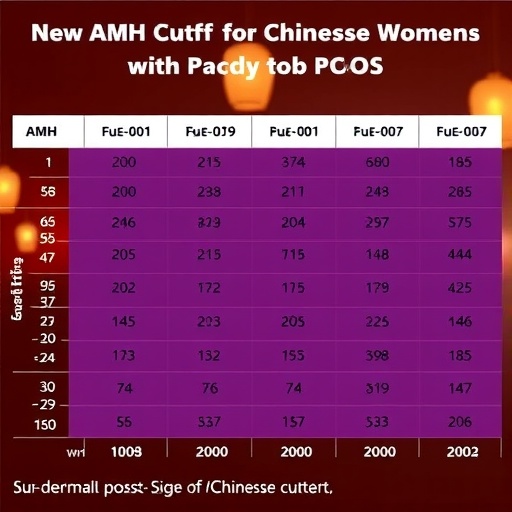
The methodology employed by the authors stands as a hallmark of well-designed epidemiological research. By using propensity score matching, the researchers were able to ensure that the results were less influenced by confounding factors that often plague observational studies. This technique involved creating pairs of subjects (one with and one without PCOS) who shared similar characteristics, thus allowing for a more precise comparison with respect to AMH levels at various ages.
As the study unfolds, readers will learn not only about the established cutoffs but also the implications these cutoffs have on clinical practice. Establishing appropriate thresholds for AMH can drastically affect treatment decisions regarding fertility and can direct how clinicians approach the management of PCOS. A more informed understanding of AMH levels enables healthcare providers to better counsel patients regarding their reproductive health and possible fertility treatment options.
The ability to segment AMH reference ranges by age is particularly crucial. Women of different ages respond differently to treatment interventions, and their ovarian response can vary significantly depending on their age group. By tailoring AMH cutoffs to specific age brackets, clinicians may ultimately improve patient outcomes through more personalized care that recognizes the biological variations inherent to different stages of life.
Furthermore, the implications of this research extend beyond individual clinical practice. On a broader scale, the establishment of standardized AMH cutoffs in different populations can contribute to a more comprehensive understanding of PCOS. This could pave the way for future research that examines how genetic, environmental, and cultural factors influence hormonal profiles and reproductive health outcomes.
While the specific data and results gleaned from the study are crucial, it is equally important to consider the limitations and areas for future research highlighted by the authors. For example, factors such as socioeconomic status, lifestyle choices, and genetic predispositions could further influence AMH levels. Future investigations may seek to explore these dimensions in depth, providing a more holistic view of ovarian health among women with PCOS.
Moreover, as scientists and clinicians work to establish better screening tools like AMH, it is essential to consider how these findings can be translated into actionable educational resources for patients. Women diagnosed with PCOS often experience feelings of isolation and anxiety regarding their reproductive futures. By providing clear, evidence-based information regarding AMH levels and their implications, healthcare providers can empower these patients to take control of their health journeys.
The study’s findings are particularly timely and relevant in the context of rising rates of PCOS diagnoses globally. As awareness and understanding of the disorder grow, so does the demand for effective screening methods that cater to varying populations’ needs. Research like that of Wang et al. stands at the forefront of this movement, representing hope for better management of PCOS and improved reproductive outcomes.
In conclusion, this retrospective study not only contributes to the body of knowledge surrounding AMH screening cutoffs for women with PCOS but also underscores the importance of age-specific evaluations in reproductive medicine. As research continues to evolve, considerations around ethnic and cultural differences will further enrich the dialogue surrounding PCOS, enabling the scientific community to tailor interventions that are both effective and empathetic.
The potential of AMH as a marker for ovarian reserve in women living with PCOS continues to be an area ripe for exploration. Researchers, healthcare providers, and patients alike should remain engaged with ongoing developments in this field to support informed decision-making regarding fertility and overall health. This study is a significant step toward a more nuanced understanding of PCOS and its management, promising to enhance the quality of care offered to countless women affected by this complex syndrome.
Subject of Research: Anti-Müllerian Hormone screening cutoffs in Chinese women with PCOS.
Article Title: Establishment of age-related AMH screening cutoffs in Chinese women with PCOS: a retrospective study using propensity score matching analysis.
Article References:
Wang, Z., Teng, X., Liu, Y. et al. Establishment of age-related AMH screening cutoffs in Chinese women with PCOS: a retrospective study using propensity score matching analysis. BMC Endocr Disord 25, 153 (2025). https://doi.org/10.1186/s12902-025-01975-4
Image Credits: AI Generated
DOI: 10.1186/s12902-025-01975-4
Keywords: AMH, PCOS, screening cutoffs, reproductive health, propensity score matching.
Tags: age-specific AMH levelsAMH cutoffs for PCOS in Chinese womenendocrinology advancementsglycoprotein hormone AMHhormonal imbalance in womeninsulin resistance in PCOSovarian function biomarkersovarian reserve assessmentPCOS complications and treatmentspolycystic ovary syndrome researchpropensity score matching analysisreproductive health challenges in PCOS