In a groundbreaking study published in the prestigious journal JAMA Network Open, researchers have cast significant doubts on the efficacy of insurance policies aimed at increasing supplemental breast cancer screening among Black women based on breast density alone. The study’s findings suggest that these well-intentioned policies may offer limited improvements in the early detection of breast cancer within this demographic, urging a reexamination of current screening protocols and multifaceted approaches that extend beyond breast density metrics.
Breast density has long been recognized as a critical factor influencing the sensitivity of mammographic cancer screening. Dense breast tissue can obscure tumors on mammograms, leading to higher rates of missed diagnoses during routine screening. As a result, supplemental imaging methods such as ultrasound or magnetic resonance imaging (MRI) have been advocated for women with dense breasts to enhance early detection rates. However, the racial disparities embedded in breast cancer incidence and outcomes complicate this narrative, particularly for Black women, who statistically face higher mortality despite similar or lower breast density averages compared to their white counterparts.
The research team, led by Dr. Anne Marie McCarthy from the University of Pennsylvania, embarked on an analytical journey to interrogate whether insurance mandates covering supplemental screening based solely on breast density criteria could significantly alter early detection landscape for Black women. Their comprehensive analysis utilized a robust dataset incorporating diverse demographic profiles, screening histories, and tumor characteristics to unravel the interplay between breast density, screening practices, and detection timing.
.adsslot_cnamjsxLdk{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_cnamjsxLdk{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_cnamjsxLdk{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
One of the pivotal revelations of the study was that although breast density remains a valuable indicator of mammography performance, its predictive utility does not translate uniformly across racial groups. For Black women, factors beyond density—such as tumor biology, genetic predispositions, and access to high-quality healthcare—exert disproportionate influence on detection outcomes. Consequently, policies that narrowly focus on breast density as the linchpin for supplemental screening eligibility may inadvertently perpetuate systemic gaps in healthcare equity.
Moreover, the research elucidated how supplemental screening modalities perform differently across racial lines. While supplemental ultrasound and MRI have demonstrated improved detection rates in women with dense breasts generally, the incremental benefit for Black women appeared muted when contextualized against their baseline risk and tumor characteristics. This nuanced insight challenges the prevailing assumption that a one-size-fits-all policy based on breast density thresholds can adequately address racial disparities in breast cancer outcomes.
The study’s methodology employed advanced statistical modeling and stratified analyses to parse out the relative contributions of breast density and other clinical variables to early cancer detection. These models accounted for confounders including age, socioeconomic status, and healthcare access, offering a multidimensional perspective on screening effectiveness. Such rigorous analytical frameworks underscore the complexity inherent in designing equitable and impactful breast cancer screening policies.
Clinically, this study serves as a clarion call to expand screening criteria and prevention strategies beyond density parameters. It advocates integrating genetic risk profiling, tumor biological markers, and social determinants of health into screening guidelines. Tailored approaches that harness emerging technologies and personalized medicine could bridge the detection gap and meaningfully improve prognosis for Black women, who disproportionately bear the mortality burden of breast cancer.
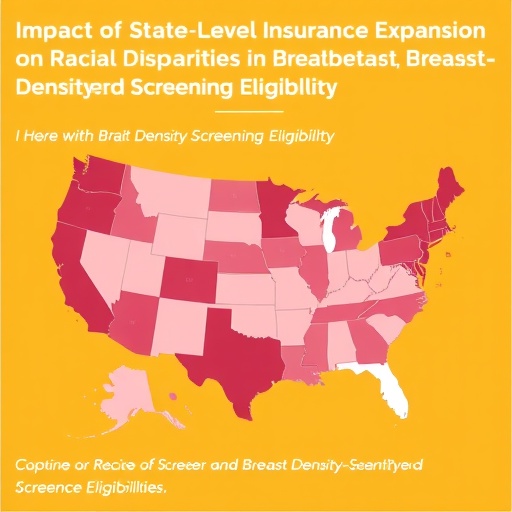
Public health implications arising from these findings are profound. Insurance coverage policies, often shaped by standardized metrics such as breast density, must evolve to embrace a more holistic understanding of cancer risk and detection efficacy. Stakeholders including policymakers, clinicians, and patient advocacy groups must collaborate to develop frameworks that reflect the multifactorial nature of breast cancer disparities.
In addition, the study highlights the urgent need for enhancing healthcare infrastructure and access in underserved communities. Even the most advanced screening technologies cannot fulfill their potential without equitable availability, culturally competent patient education, and adherence support systems. Investment in community health initiatives and targeted outreach must accompany policy reforms for tangible impact.
It is also noteworthy that the study refrains from discounting the role of breast density entirely but situates it within a broader context. This nuanced stance invites a recalibration of screening strategies to prioritize individualized risk assessment over blanket policy applications. Precision medicine approaches that integrate comprehensive risk modeling may supersede density-based mandates, promoting earlier detection and better clinical outcomes.
Furthermore, the authors emphasize ongoing research to decode the unique tumor biology observed in Black women, which may elucidate mechanisms underlying the observed disparity in screening efficacy. Molecular and genetic investigations, coupled with epidemiologic studies, will be instrumental in crafting next-generation screening paradigms that are sensitive to racial and biological heterogeneity.
The implications of this study resonate beyond breast cancer screening into the larger discourse on health equity and evidence-based policy. It exemplifies how nuanced data analysis can challenge prevailing medical dogma and catalyze improved care standards. As science uncovers layers of complexity in disease presentation and detection, healthcare systems must adapt flexibly and inclusively to serve diverse populations effectively.
In conclusion, the investigation led by Dr. McCarthy signals a pivotal turning point in breast cancer screening policy discourse. It underscores the limitations of relying solely on breast density to guide supplemental screening insurance coverage, particularly for Black women. This insight paves the way for innovation in personalized screening strategies that comprehensively address racial disparities, ultimately striving toward equitable early cancer detection and improved survival outcomes.
Subject of Research: Breast cancer screening efficacy and racial disparities, with a focus on the impact of breast density-based supplemental screening coverage for Black women.
Article Title: Not provided in the source content.
News Publication Date: Not provided in the source content.
Web References: Not provided in the source content.
References: (doi:10.1001/jamanetworkopen.2025.25216)
Image Credits: Not provided in the source content.
Keywords: Breast cancer, Racial differences
Tags: breast density and screening eligibilityDr. Anne Marie McCarthy research analysisearly detection of breast cancerefficacy of insurance policies in healthcarehealth equity in breast cancer outcomesimpact of breast density on cancer diagnosisJAMA Network Open study findingsmammography limitations for dense breastsmultifaceted approaches to breast cancer screeningracial disparities in breast cancer screeningstate-level insurance expansionsupplemental breast cancer screening for Black women