A groundbreaking study published in BMC Cancer introduces a sophisticated nomogram that integrates body composition and tumor burden indicators to accurately predict lymph node metastasis (LNM) in patients diagnosed with T1 esophageal squamous cell carcinoma (ESCC). This novel approach promises to revolutionize the clinical decision-making process in early esophageal cancer management by providing a precise, individualized risk assessment tool that outperforms traditional predictive parameters.
Lymph node metastasis remains a formidable hurdle in the treatment and prognosis of early-stage esophageal cancer. Despite advancements in imaging and pathological techniques, clinicians continue to face challenges in reliably identifying patients at high risk of metastasis. The complexity of tumor biology coupled with individual variations in patient physiology necessitates innovative solutions that extend beyond conventional metrics.
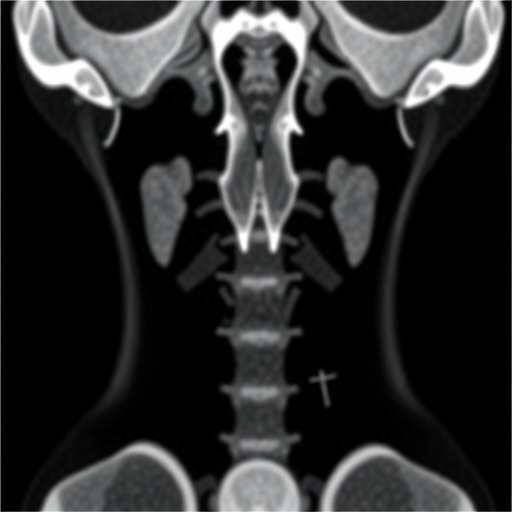
The recently developed nomogram leverages detailed body composition analysis obtained from computed tomography (CT) images, focusing particularly on the quantification of skeletal muscle, subcutaneous fat, and visceral fat around the lumbar 3 (L3) vertebra, an anatomical landmark frequently utilized for such assessments. By integrating these parameters with tumor burden characteristics like size, lymphovascular invasion (LVI), and tumor staging, the model offers a multidimensional perspective on metastatic potential.
.adsslot_oVJpN175ne{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_oVJpN175ne{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_oVJpN175ne{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The researchers conducted a robust retrospective analysis of clinical and imaging data from 243 patients with histologically confirmed T1 ESCC who underwent radical surgical procedures. Utilizing ImageJ software, the team meticulously measured cross-sectional areas of relevant tissues in the L3 region. This comprehensive dataset enabled a nuanced exploration of the relationship between host body composition and cancer progression.
Through rigorous univariate and subsequent multivariate statistical analyses, several independent predictors of lymph node metastasis emerged. Tumor size and lymphovascular invasion reaffirmed their established roles as significant risk factors. Notably, visceral fat area (VFA) and substage classification within T1 also surfaced as critical determinants, highlighting the influence of both tumor biology and patient metabolic status on metastatic behavior.
The predictive power of these individual factors was quantified using receiver operating characteristic (ROC) curve analyses, revealing moderate discriminative abilities when considered in isolation. For instance, the area under the curve (AUC) for VFA reached 0.767, demonstrating a considerable association between visceral adiposity and LNM risk. However, none of the single indicators achieved the level of accuracy desired for clinical application on their own.
Integration into a nomogram markedly enhanced predictive performance. The composite model incorporating tumor size, LVI, VFA, and T1 substage exhibited an impressive AUC of 0.8331 in the training cohort and 0.8343 upon external validation. These values underscore the enhanced prognostic accuracy afforded by fusing tumor characteristics with patient-specific body composition metrics, bolstering its clinical utility.
Calibration plots affirmed the nomogram’s reliability by demonstrating strong concordance between predicted and observed lymph node metastasis rates. Moreover, decision curve analysis (DCA) highlighted its potential to improve clinical outcomes, suggesting that utilizing this tool could optimize therapeutic strategies by refining patient risk stratification and informing tailored intervention plans.
The study’s emphasis on visceral fat is particularly noteworthy. Visceral adiposity, distinguished metabolically from subcutaneous fat, is increasingly recognized for its role in modulating tumor microenvironments and systemic inflammatory responses. Elevated VFA may contribute to a pro-tumorigenic milieu, facilitating not only local invasion but also distant metastatic spread through lymphatic routes.
Similarly, the incorporation of the T1 substage further refines the model. Substaging reflects the depth of tumor invasion within the esophageal wall layers, which is intrinsically linked to metastatic potential. This granular staging captures subtle variations in tumor behavior that overarching T-category classifications may overlook.
This research marks a significant step toward precision oncology in esophageal cancer care. By providing an accessible, CT-based nomogram, clinicians can better discriminate which patients harbor occult lymph node metastases, thereby guiding decisions regarding the extent of surgical intervention, neoadjuvant therapy, or vigilant surveillance.
Importantly, the nomogram’s reliance on routinely obtained preoperative imaging ensures its adaptability across diverse healthcare settings without necessitating additional costly or invasive testing. Its quantitative foundation also facilitates objective risk stratification, minimizing subjective interpretation that can cloud treatment planning.
Furthermore, this tool aligns with the broader shift in oncology toward integrating host factors, such as nutritional and metabolic status, into cancer prognosis models. Recognizing that patient physiology intricately influences tumor progression amplifies the need for multidimensional prediction frameworks like the one proposed.
Looking ahead, prospective studies validating this nomogram across larger, multi-center cohorts will be vital to establish its generalizability and refine its parameters. Integrating molecular biomarkers alongside imaging-derived body composition indices might further enhance accuracy, blending phenotypic and genotypic insights.
In conclusion, this innovative nomogram developed by Liu and colleagues represents a pivotal advancement in predicting lymph node metastasis for patients with T1 esophageal squamous cell carcinoma. By marrying tumor burden indicators with host body composition factors, it transcends traditional prognostic models, offering a dynamic and individualized predictive tool poised to impact clinical outcomes profoundly.
Subject of Research: Development of a predictive nomogram combining body composition and tumor burden indicators to assess lymph node metastasis in T1 esophageal squamous cell carcinoma.
Article Title: Development of a nomogram based on body composition and tumor burden indicators to predict lymph node metastasis in patients with T1 esophageal squamous cell carcinoma.
Article References:
Liu, Q., Hu, J., Liu, L. et al. Development of a nomogram based on body composition and tumor burden indicators to predict lymph node metastasis in patients with T1 esophageal squamous cell carcinoma. BMC Cancer 25, 1266 (2025). https://doi.org/10.1186/s12885-025-14703-x
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14703-x
Tags: advanced imaging techniques in oncologybody composition analysis in cancercomputed tomography in cancer diagnosisearly esophageal cancer managementinnovative solutions for cancer prognosislymph node metastasis predictionlymphovascular invasion in esophageal cancernomogram for cancer risk assessmentpersonalized cancer treatment strategiesretrospective analysis of cancer dataT1 esophageal squamous cell carcinomatumor burden indicators in esophageal cancer