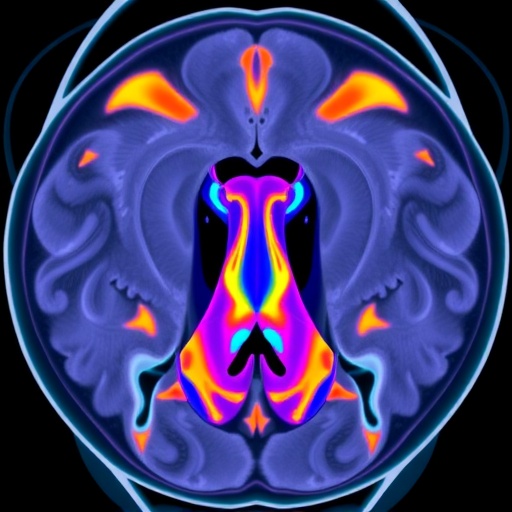
Advancements in medical imaging technologies continue to revolutionize cancer treatment strategies, offering clinicians enhanced tools to improve therapeutic outcomes while minimizing adverse effects. Recently, a novel MRI technique known as the enhanced 3D-NEVERview + C sequence has demonstrated promising clinical benefits in the radiotherapy planning process for patients suffering from nasopharyngeal carcinoma (NPC) with cervical lymph node metastasis. This breakthrough imaging approach is poised to significantly refine the accuracy of tumor and critical structure delineation, potentially transforming radiotherapy protocols.
Nasopharyngeal carcinoma remains a challenging malignancy due to its anatomical complexity and proximity to vital neurovascular structures such as the brachial plexus. Radiotherapy is a cornerstone in NPC treatment, but the risk of radiation-induced nerve injury necessitates meticulous planning. Recent research spearheaded by Li et al. introduces the enhanced 3D-NEVERview + C MRI sequence, which elevates the visualization of the brachial plexus during simulation, thereby improving dose sparing of this critical structure.
Traditional MRI sequences often struggle with precise delineation of the brachial plexus due to low contrast and indistinct boundaries in the complex cervical region. The 3D-NEVERview + C sequence employs an augmented contrast agent combined with advanced imaging parameters to optimize the contrast-to-noise ratio (CNR), signal-to-noise ratio (SNR), and contrast ratio (CR). This enhancement facilitates the clear visualization of nerve bundles, which is vital for targeted radiotherapy.
.adsslot_29l7RFjWXu{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_29l7RFjWXu{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_29l7RFjWXu{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The study enrolled fifty NPC patients exhibiting cervical lymph node metastasis, a demographic notably susceptible to brachial plexus exposure. The researchers meticulously compared imaging metrics between the new 3D-NEVERview + C sequence and conventional MRI protocols. Quantitative analyses revealed statistically significant improvements across all imaging quality parameters, emphasizing the sequence’s superior capacity for nerve visualization.
Beyond imaging quality, an essential component of this investigation focused on the volumetric assessment of the brachial plexus. Automated and manual delineations of nerve volumes were performed, exposing marked discrepancies between methods but importantly validating the enhanced sequence’s ability to capture more detailed anatomy. The automatically determined volumes using the 3D-NEVERview + C were consistently smaller yet more precise, reflecting an improved delineation threshold.
Radiotherapy planning incorporated evaluations of dose-volume histograms (DVH), contrasting original plans without brachial plexus constraints against optimized plans integrating dose limitations. The comparative dosimetry exhibited significant reductions in the volumes of brachial plexus receiving high-dose radiation (V60 and V66) and notable decreases in maximum (Dmax) and mean doses (Dmean). These findings underscore the clinical relevance of enhanced imaging in protecting nerve function.
The implications of these dose reductions extend beyond imaging metrics, as sparing the brachial plexus can markedly diminish the risk of radiation-induced brachial plexopathy, a debilitating nerve injury syndrome characterized by pain, weakness, and sensory loss. Historically, overexposure of this structure has complicated NPC radiotherapy, thereby compelling the development of imaging tools that promote safer treatment paradigms.
Incorporating the 3D-NEVERview + C sequence into routine MRI simulation (MRI-sim) protocols represents a paradigm shift. It not only refines the anatomical mapping of the brachial plexus but also enables radiation oncologists to tailor treatment plans with enhanced precision, balancing oncologic control with neuroprotection. This advancement aligns with the broader goals of precision oncology and personalized medicine.
It is pertinent to recognize that the enhanced contrast achieved by the 3D-NEVERview + C hinges on sophisticated imaging technology, relying on paramagnetic contrast agents and optimized pulse sequences to amplify nerve-tissue differentiation. This allows clinicians to discern critical structures that were previously indistinguishable against surrounding tissues, thereby reducing uncertainties in contouring and planning.
Furthermore, the study’s methodology exemplifies rigorous statistical validation, strengthening confidence in the reproducibility and applicability of findings across clinical settings. By demonstrating statistically significant improvements (p<0.05) in imaging parameters and dosimetric outcomes, the research lays the groundwork for longitudinal studies assessing patient quality of life and long-term neurological outcomes.
Given the anatomical challenges inherent to NPC, particularly in cases with nodal metastasis, the enhanced visualization capabilities provided by the 3D-NEVERview + C have the potential to influence decisions beyond radiotherapy. For instance, surgical planning and diagnostic assessments may also benefit from the improved nerve mapping, fostering multidisciplinary integration.
The safety profile of the contrast agents utilized in the 3D-NEVERview + C sequence remains a consideration, but current evidence indicates acceptable tolerability in oncologic imaging. Continued evaluation of contrast media effects will ensure patient safety remains paramount as these advanced imaging techniques become standard practice.
Looking forward, the integration of this enhanced MRI sequence with emerging artificial intelligence-powered segmentation tools may usher in an era of automated, high-precision delineations, drastically reducing inter-observer variability and accelerating clinical workflows. Such developments could further enhance the therapeutic ratio in NPC management.
In conclusion, the research highlights the critical role of advanced imaging in optimizing radiotherapy for nasopharyngeal carcinoma. The enhanced 3D-NEVERview + C sequence significantly augments brachial plexus visualization, enabling clinicians to implement dose constraints effectively and potentially reduce nerve injury risk. This innovation exemplifies the intersection of imaging technology and clinical oncology, heralding improved patient outcomes.
As the oncologic community strives to mitigate treatment-related morbidities while maximizing tumor control, adopting advanced MRI sequences such as the 3D-NEVERview + C may become the new standard. Its ability to furnish clearer anatomical details paves the way for safer, more effective radiotherapy interventions in challenging head and neck cancers.
The study serves as a compelling call to action for institutions employing MRI simulation in radiotherapy planning, underscoring the necessity of updating imaging protocols to harness technological advancements. Through multidisciplinary collaboration and continued research, these scientific strides can translate into tangible benefits for patients worldwide.
With radiotherapy techniques continuously evolving through technological innovations, the enhanced 3D-NEVERview + C sequence represents a leap forward in precision imaging. This not only underscores the value of investing in cutting-edge MRI technologies but also reinforces the commitment to improving the therapeutic index for NPC patients under complex treatment regimens.
Ultimately, this work exemplifies how targeted imaging improvements can ripple across the entire treatment continuum, from planning to execution, reducing complications while preserving vital neurological function. The enhanced 3D-NEVERview + C sequence is poised to become an indispensable tool in the fight against nasopharyngeal carcinoma.
Subject of Research: Clinical evaluation of an enhanced MRI sequence (3D-NEVERview + C) for improved radiotherapy planning in nasopharyngeal carcinoma patients with cervical lymph node metastasis, focusing on brachial plexus delineation and dose reduction.
Article Title: Clinical benefits of enhanced 3D-NEVERview sequence in MRI simulation for nasopharyngeal carcinoma patients received radiotherapy.
Article References:
Li, Y., Zhang, Y., Tang, R. et al. Clinical benefits of enhanced 3D-NEVERview sequence in MRI simulation for nasopharyngeal carcinoma patients received radiotherapy. BMC Cancer 25, 1232 (2025). https://doi.org/10.1186/s12885-025-14695-8
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14695-8
Tags: 3D-NEVERview MRI techniquebrachial plexus visualizationcancer treatment advancementscervical lymph node metastasis radiotherapyenhanced medical imaging technologiesMRI contrast optimization strategiesnasopharyngeal carcinoma imagingnovel imaging approaches in oncologyprecision in cancer imagingradiation-induced nerve injury preventionradiotherapy planning for NPCtumor delineation in radiotherapy