In the evolving landscape of oncological surgery, the management of retroperitoneal vascular leiomyosarcoma (RVLMS) remains an exceptional challenge. RVLMS, a rare malignancy deriving from the smooth muscle cells of vascular walls, predominantly affects the inferior vena cava (IVC), compelling surgeons to devise intricate strategies for successful resection and reconstruction. A recent comprehensive study led by Yang et al., published in BMC Cancer (2025), sheds new light on the imaging-based classification of RVLMS and how it can inform surgical decision-making to improve patient outcomes. This investigation, conducted at a single medical center, spans nearly a decade, providing crucial insights into operative management and postoperative prognosis.
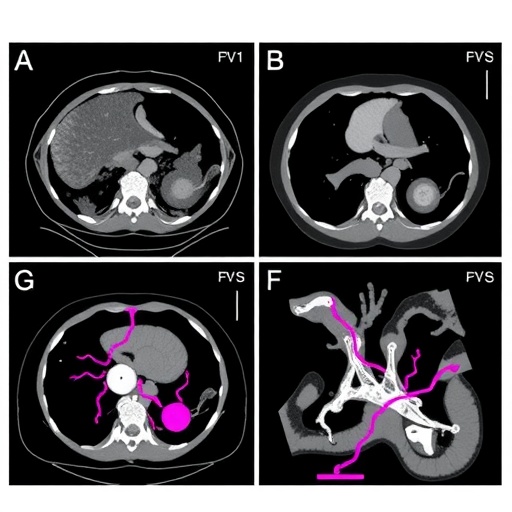
Retroperitoneal tumors, because of their deep anatomical location and proximity to vital structures like the IVC, pose considerable technical difficulties for surgeons aiming for curative resection. RVLMS falls into this category, with a tendency for both intraluminal growth and extraluminal extension, often distorting the vascular architecture. The study underscores an imaging classification system stratifying RVLMS into four distinct types: intraluminal, intermediate, extraluminal, and peripheral. Each classification corresponds to tumor involvement patterns in relation to the IVC, guiding surgeons in anticipating operative complexity and tailoring vascular reconstruction approaches accordingly.
The intraluminal type encompasses tumors primarily confined within the lumen of the IVC, posing a significant risk of vascular obstruction and thrombotic complications. Intermediate types exhibit combined features of intraluminal and extraluminal extension. Extraluminal tumors localize primarily outside the vessel but often adhere closely to the vascular wall, while peripheral types are situated somewhat distally, involving peripheral veins with relatively sparing of the main caval structure. This nuanced categorization emerges as a pivotal tool not only in preoperative planning but also in predicting intraoperative challenges such as blood loss and operative duration.
.adsslot_42f1Bm5Wuc{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_42f1Bm5Wuc{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_42f1Bm5Wuc{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Quantitative data from 24 patients who underwent primary RVLMS resection between 2015 and 2023 reveal a median tumor size of 80 millimeters, reflecting the often insidious, late presentation of these tumors. Surgical times averaged nearly five hours, with substantial variability attributable to tumor classification. Notably, patients with intermediate and intraluminal types tended to experience longer operative times and increased blood loss compared to those with extraluminal and peripheral tumors, highlighting the impact of tumor-vessel interface on surgical morbidity.
Vascular reconstruction techniques varied per the type and extent of tumor involvement. Primary repair was the most commonly employed method in 15 cases, emphasizing conservative restoration of IVC integrity. Patch angioplasty, applied in two patients, employed graft materials to reconstruct segmented vessel walls, while four cases involved ligation of the inferior vena cava, a measure reserved for extensive tumor involvement when reconstruction was unfeasible or contraindicated. These surgical decisions stem from intricate preoperative imaging assessments combined with intraoperative judgment balancing oncological clearance against vascular preservation.
Margin status remains one of the cornerstones of oncologic surgery, and in this cohort, three patients experienced R1 or R2 resections, indicating microscopic or macroscopic residual tumor presence respectively. While complete resection with negative margins is paramount for long-term disease control, the anatomical complexities of RVLMS sometimes preclude radical excision, underscoring the importance of individualized surgical planning bolstered by robust imaging data.
Postoperative outcomes mirrored the inherent aggressiveness of RVLMS. With a median follow-up nearing one year, approximately 21% of patients experienced local recurrence, and nearly 29% developed distant metastases. One individual presented with both local and distant disease progression, illuminating the dual challenges of local tumor control and systemic dissemination intrinsic to sarcomatous malignancies. The median disease-free survival reached 19 months, a metric that, while modest, validates the role of surgical intervention complemented by vigilant follow-up.
The study’s revelations about the correlation between imaging classification and surgical complexity are profound. Surgeons can anticipate extended operative times and greater transfusion requirements in patients harboring intraluminal and intermediate tumor types, allowing for preoperative optimization of resources and multidisciplinary collaboration. This stratification fosters personalized surgery, potentially mitigating perioperative risks and enhancing recovery trajectories.
Moreover, the findings advocate for a paradigm shift in RVLMS management, where imaging not only serves diagnostic purposes but also prognostic and strategic roles. Advanced modalities such as contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) afford detailed visualization of tumor-vessel relationships, vascular wall infiltration, and collateral circulation, thereby shaping surgical approaches ranging from conservative vascular repair to definitive ligation.
The broader oncological community stands to benefit from these insights, particularly in centers managing complex retroperitoneal sarcomas. The retrospective study’s depth offers a template for refining surgical curricula, encouraging incorporation of imaging classifications into multidisciplinary tumor boards and fostering innovation in reconstructive vascular surgery.
Looking forward, the authors emphasize the importance of longer follow-up periods and larger multicentric cohorts to validate and expand these findings. The integration of molecular profiling and targeted therapies could further customize treatment pathways alongside surgical intervention, potentially improving survival rates.
This pioneering exploration into RVLMS surgical strategy marks a significant advancement, bridging radiological evaluation with operative management to confront a challenging malignancy. As imaging techniques evolve and surgical expertise advances, patients afflicted with RVLMS may anticipate more tailored, effective interventions rooted in comprehensive preoperative assessment.
In conclusion, Yang et al.’s study offers a pivotal framework reconciling imaging classification with surgical strategy for RVLMS, underscoring the essential interplay between diagnostic precision and surgical prowess. This approach not only enhances therapeutic outcomes but also provides a roadmap for future research and clinical protocol development in the management of rare vascular sarcomas of the retroperitoneum.
Subject of Research: Retroperitoneal vascular leiomyosarcoma (RVLMS) imaging classification and surgical strategy.
Article Title: Imaging classification and surgical strategy of retroperitoneal vascular leiomyosarcoma: experience from a single medical center.
Article References:
Yang, B., Zhao, X., Wang, G. et al. Imaging classification and surgical strategy of retroperitoneal vascular leiomyosarcoma: experience from a single medical center. BMC Cancer 25, 1241 (2025). https://doi.org/10.1186/s12885-025-14287-6
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14287-6
Tags: challenges in oncological surgerycomprehensive studies in cancer managementimaging-based classification of tumorsinferior vena cava tumor resectioninsights into retroperitoneal tumorsintraluminal tumor growth patternspostoperative prognosis for leiomyosarcomarare malignancies and surgical challengesretroperitoneal vascular leiomyosarcomasurgical decision-making in oncologysurgical management of RVLMSvascular reconstruction techniques