A groundbreaking study has recently emerged from the surgical oncology community, shedding new light on reconstruction techniques following proximal gastrectomy (PG). Researchers have conducted an in-depth evaluation comparing a novel surgical technique named modified tubular esophagogastrostomy (mTEG) with the more established double tract reconstruction (DTR). This comparative analysis not only hopes to influence surgical choice but also aspires to optimize patient recovery and postoperative quality of life, which remains a pivotal concern in gastric surgery.
Proximal gastrectomy is a critical surgical intervention for patients with tumors located in the upper stomach, where removal of part of the stomach is necessary. The challenge post-surgery lies in reconstructing the gastrointestinal tract in a way that minimizes reflux, preserves nutrition, and ensures a swift recovery. While double tract reconstruction has been a traditional choice, the mTEG approach presents a technically refined alternative, promising enhanced outcomes without compromising safety.
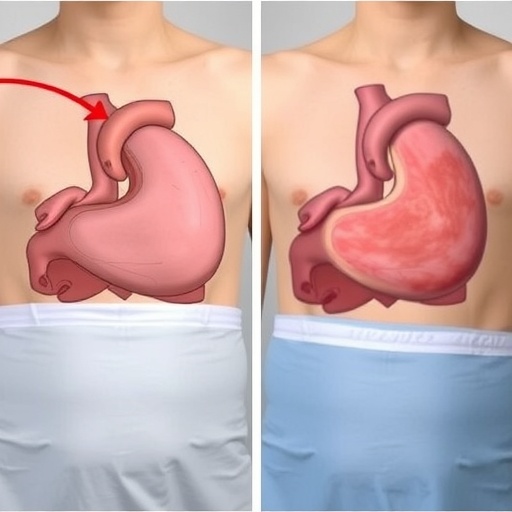
The modified tubular esophagogastrostomy technique is a sophisticated surgical procedure comprising three pivotal components. First, it involves a tubular reconstruction of the gastric remnant, essentially reshaping the remaining stomach tissue into a tubular form to facilitate better functional connectivity. The second step is the creation of a 3-centimeter artificial gastric fornix. This anatomical modification aims to mimic the natural reservoir function of the stomach, crucial for food storage and gradual release. Lastly, the procedure enhances the His angle—the acute angle at the esophagogastric junction—by sharpening it alongside posterior mediastinal fixation, mechanisms that collectively help reduce reflux incidence.
This retrospection-based study incorporated 288 patients who underwent proximal gastrectomy between 2021 and 2024. Using propensity score matching, a statistical matching technique to balance baseline clinical variables between groups, the researchers analyzed 33 matched pairs, ensuring a scientifically robust and fair comparison. Parameters such as operative time, postoperative complications, nutritional status, and quality of life were meticulously investigated, providing a comprehensive overview of the comparative efficacy of mTEG and DTR.
Significantly, the mTEG technique demonstrated substantial advantages in surgical efficiency. Median operative time was dramatically reduced to 163.7 minutes compared to 247.9 minutes for the double tract procedure. This nearly one-hour difference in operating room duration not only optimizes healthcare resources but potentially decreases anesthesia-related risks for patients. Additionally, the postoperative hospital stay was shorter for mTEG recipients, averaging 8.3 days as opposed to 9.9 days in the DTR cohort, indicating faster convalescence and lowered hospitalization costs.
Intraoperative metrics such as estimated blood loss and the number of lymph nodes retrieved during surgery were comparable between the two groups, illustrating that the mTEG method does not compromise oncologic thoroughness or patient safety. These factors are vital as they assure surgeons that oncological principles remain uncompromised despite procedural innovation.
When evaluating early postoperative complications, a revealing difference manifested. All observed early complications, including two cases of anastomotic leakage, one chylous leakage, and a pulmonary-related complication, occurred exclusively in the DTR group. The mTEG group encountered no such issues during the critical first 30 days after surgery. Although complication rates did not reach statistical significance, this trend underscores the potential of mTEG to minimize early postoperative morbidity, an essential consideration in surgical planning.
Another critical concern after proximal gastrectomy is the risk of reflux esophagitis, a painful condition where stomach acid flows back into the esophagus, potentially leading to severe tissue damage. Endoscopic evaluation revealed comparable rates of reflux esophagitis graded as Los Angeles B or higher between mTEG (11.1%) and DTR (4.5%) patients, with no significant statistical difference. This finding confirms that mTEG does not elevate reflux risk despite its novel reconstructive design.
Nutritional outcomes are paramount after gastric surgeries since malnutrition can significantly affect recovery and longer-term health. The research team assessed multiple indicators, including serum prealbumin, albumin, hemoglobin levels, and body mass index at 1, 3, and 6 months post-surgery. Both mTEG and DTR groups exhibited similar nutritional profiles without significant differences, demonstrating that mTEG preserves essential nutritional status effectively.
Quality of life (QoL), often the ultimate measure of surgical success from the patient’s perspective, was assessed using the validated EORTC QLQ-STO22 questionnaire at six months postoperatively. Results indicated no discernible differences between the two groups, signaling that mTEG can match the established DTR method in maintaining patients’ perceived well-being and symptom control after surgery.
The strategic design of the mTEG technique harnesses anatomical and surgical principles to enhance functional outcomes. Tubular reshaping of the gastric remnant facilitates improved motility and reservoir function. The artificial fornix mimics physiological stomach architecture, while His angle reconstruction acts as a natural antireflux barrier. These innovations collectively contribute to maintaining esophageal protection against gastric contents, reflexively improving patient comfort.
From a surgical standpoint, the reduced operation time and hospitalization duration offered by mTEG hint at a shift toward more efficient practices that may substantially benefit both healthcare systems and patients. Less time under anesthesia can decrease intraoperative risks, while quicker discharge reduces exposure to hospital-related complications and costs.
The fact that mTEG shows equivalent nutritional outcomes without increased reflux risk or complication frequency makes it an attractive option for surgeons seeking to balance efficacy with patient-centered care. Its technical advancements may facilitate widespread adoption, especially with increasing expertise in minimally invasive gastric surgery.
This study provides critical evidence supporting mTEG as a feasible, safe, and potentially preferable reconstruction method following proximal gastrectomy. While long-term oncological outcomes and quality of life require further investigation, the favorable short-term results position mTEG as a compelling alternative to double tract reconstruction.
In summary, the evolution of gastric reconstructive surgery continues to accelerate, with modified tubular esophagogastrostomy providing a blueprint for future innovations. By integrating anatomical insight with surgical precision, this technique enhances patient outcomes while optimizing operative efficiency, heralding a new era in stomach cancer surgery.
Subject of Research: Surgical reconstruction techniques following proximal gastrectomy, comparing modified tubular esophagogastrostomy (mTEG) and double tract reconstruction (DTR).
Article Title: Safety and short‑term outcomes of a modified tubular esophagogastrostomy versus double tract reconstruction after proximal gastrectomy: a propensity score matching analysis.
Article References:
Zhang, C., Wang, K., Zhang, Z. et al. Safety and short‑term outcomes of a modified tubular esophagogastrostomy versus double tract reconstruction after proximal gastrectomy: a propensity score matching analysis. BMC Cancer 25, 908 (2025). https://doi.org/10.1186/s12885-025-14284-9
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14284-9
Tags: cancer surgery outcomesdouble tract reconstructiongastrointestinal tract reconstructionmodified tubular esophagogastrostomynovel surgical techniques comparisonnutritional preservation after surgerypatient quality of life in surgerypostoperative recovery in gastric surgeryproximal gastrectomy techniquesreflux management in gastrectomysafety in gastric reconstructionsurgical oncology advancements