Recent findings at Cold Spring Harbor Laboratory (CSHL) shine a new light on pancreatic cancer.
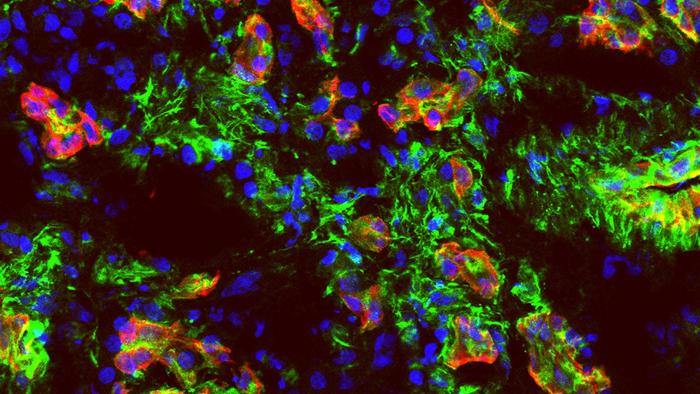
Credit: Fearon lab/Cold Spring Harbor Laboratory
Recent findings at Cold Spring Harbor Laboratory (CSHL) shine a new light on pancreatic cancer.
More than 90% of pancreatic cancer cases are attributed to an aggressive, deadly form of the disease called pancreatic ductal adenocarcinoma, or PDAC. Researchers have a poor understanding of how our immune system interacts with PDAC. So, coming up with treatments is tricky. It’s thought patients do not show a natural immune response to the cancer because the tumor environment somehow prevents that response. Many are unconvinced that PDAC interacts with the immune system at all.
CSHL scientists have now confirmed that pancreatic cancer does trigger a response in our immune system. However, the T cells that help fight off most diseases have a hard time infiltrating PDAC tumors. These findings could help guide future efforts for developing treatments.
For this study, CSHL Professor Douglas Fearon worked with a team including lead author Min Yao, Professor Matthew Weiss from the Zucker School of Medicine, and CSHL Partners for the Future program participant Sophia Shen from Cold Spring Harbor High School. They first set out to find a new antigen present only in PDAC tumors and not in normal tissue. The body makes cells called antibodies that recognize specific antigens and help destroy them. Identifying a new PDAC antigen could help explain why some patients have better outcomes than others.
The team sequenced plasma cells in pancreatic tumor samples taken from seven Northwell Health patients. They then created synthetic antibodies based on that sequence. The idea was that the synthetic antibodies would point the team toward the new PDAC antigen behind the body’s immune response. But they didn’t find the one they were looking for. Instead, they found 25 antibodies that responded to antigens from cancer cells and normal cells produced in the body. These antibodies were consistent across patients.
“I was surprised at the clarity of the data, that we had a number of antibodies react with the same antigen from multiple patients,” Fearon says.
Previously, researchers had believed that pancreatic cancer suppresses immunity. Some have even explored vaccination as a possible solution. Based on his team’s findings, Fearon says that strategy likely isn’t needed.
“Pancreatic cancer is not immunologically silent. That’s the message,” explains Fearon. “Pancreatic tumors are already immunogenic. We have a challenge in allowing the immune response to attack the cancer.”
Now that scientists better understand the problem, they can try to develop workable solutions. For the pancreatic cancer community, that’s real progress and a welcome development unto itself.
Journal
JCI Insight
DOI
10.1172/jci.insight.172449



