The American Gastroenterological Association (AGA) issues new clinical guidelines on drug therapy for the management of moderate-to-severe luminal and fistulizing Crohn’s disease.
Credit: American Gastroenterological Association
Bethesda, MD (May 27, 2021) — Crohn’s disease, a type of inflammatory bowel disease (IBD) that causes inflammation (pain and swelling) in the gastrointestinal tract, can cause daily health problems, frequent hospitalizations and surgery when not adequately controlled. While there is no cure for Crohn’s disease, there are treatments that can help patients live a symptom-free life.
After a detailed review of available literature, the American Gastroenterological Association (AGA) has released new clinical guidelines outlining the benefits and risks of each drug currently available to Crohn’s patients. Based on this research, AGA recommends the early introduction of biologics for patients experiencing luminal and fistulizing Crohn’s disease rather than waiting until other treatments fail. These guidelines are published in Gastroenterology, AGA’s official journal.
“With many new drugs entering the market, clinician’s ability to treat patients with Crohn’s disease has improved greatly over the last 20 years,” said lead author Joseph D. Feuerstein, MD, from Beth Israel Deaconess, Boston, Massachusetts. “We hope this new guideline serves as a manual for clinicians in selecting the right therapies for their patients, which should lead to improved patient outcomes and less need for invasive surgery.”
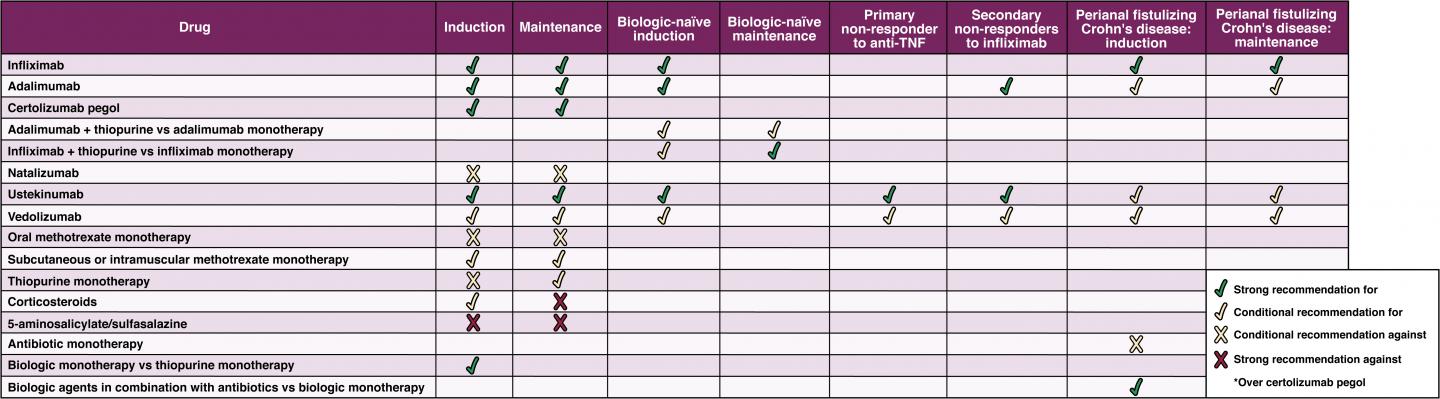
Key guideline recommendations:
- 1. Biologics are the most effective drugs for the management of Crohn’s and they should be used early, rather than delaying their use until after failure of mesalamine and/or corticosteroids, in patients with moderate to severe or fistulizing Crohn’s disease. These drugs are antibodies and can more precisely target the immune system which is causing the inflammation in Crohn’s disease.
a. Anti-tumor necrosis factor (anti-TNF) agents or ustekinumab are recommended and vedolizumab is suggested as a first-line treatment.
b. In patients who have previously not responded to anti-TNF agents, AGA recommends ustekinumab or vedolizumab.
c. The biologic natalizumab is no longer recommended due to potential adverse events and the availability of safer treatment options.
Read the AGA Clinical Practice Guideline on the Medical Management of Moderate to Severe Luminal and Fistulizing Crohn’s Disease to review all 25 recommendations.
###
Resources
Guidelines
Technical review
Spotlight (infographic)
Clinical Decision Support Tool
Commentary: Providing the Best Care for Patients with Crohn’s Disease: An Examination of the New AGA Clinical Practice Guideline on the Medical Management of Moderate to Severe Luminal and Fistulizing Crohn’s Disease
Media contact: Courtney Reed, [email protected], 301-272-0025
About the AGA Institute
The American Gastroenterological Association is the trusted voice of the GI community. Founded in 1897, the AGA has grown to more than 16,000 members from around the globe who are involved in all aspects of the science, practice and advancement of gastroenterology. The AGA Institute administers the practice, research and educational programs of the organization. http://www.
AGA is now on Instagram.
Like AGA on Facebook.
Follow us on Twitter @AmerGastroAssn.
Check out our videos on YouTube.
Join AGA on LinkedIn.
Media Contact
Courtney Reed
[email protected]