Credit: Liming Cheng, Rongrong Zhu, Department of Orthopedics, Tongji Hospital of Tongji University
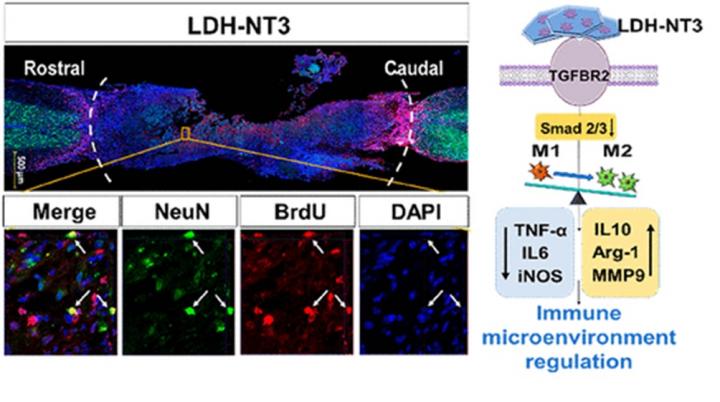
Researchers from the Department of Orthopedics of Tongji Hospital at Tongji University in Shanghai have successfully used a nanobiomaterial called layered double hydroxide (LDH) to inhibit the inflammatory environment surrounding spinal cord injuries in mice, accelerating regeneration of neurons and reconstruction of the neural circuit in the spine. The researchers were also able to identify the underlying genetic mechanism by which LDH works. This understanding should allow further modification of the therapy which, in combination with other elements, could finally produce a comprehensive, clinically applicable system for spinal cord injury relief in humans.
The research appears in the American Chemical Society journal ACS Nano on February 2.
There is no effective treatment for spinal cord injuries, which are always accompanied by death of neurons, breakage of axons, or nerve fibers, and inflammation. Even though new neural stem cells continue to be generated by the body, this inflammatory microenvironment (the immediate, small-scale conditions at the injury site) severely hinders regeneration of neurons and axons. Worse still, the prolonged activation of immune cells in this area also results in secondary lesions of the nervous system, in turn preventing the stems cells from differentiating themselves into new cell types.
If this aggressive immune response at the injury site could be moderated, there is the possibility that neural stem cells could begin differentiation and neural regeneration could occur.
Image title: Nanobiomaterial boosts neuronal growth in mice
Image caption: Researchers from the Department of Orthopedics of Tongji Hospital have successfully used a nanobiomaterial called layered double hydroxide (LDH) to inhibit the inflammatory environment surrounding spinal cord injuries in mice, accelerating regeneration of neurons and reconstruction of the neural circuit in the spine.
Image credit: Liming Cheng, Rongrong Zhu, Department of Orthopedics, Tongji Hospital of Tongji University
Image usage restrictions: News organizations may use or redistribute this image, with proper attribution, as part of news coverage of this paper only.
In recent years, a raft of novel nano-scale biomaterials — natural or synthetic materials that interact with biological systems — have been designed to assist activation of neural stem cells, along with their mobilization and differentiation. Some of these “nanocomposites” are capable of delivering drugs to the injury site and accelerate neuronal regeneration. These nanocomposites are especially attractive for spinal cord treatment due to their low toxicity. However, few have any ability to inhibit or moderate the immune reaction at the site, and so do not tackle the underlying problem. Moreover, the underlying mechanisms of how they work remains unclear.
Nanolayered double hydroxide (LDH) is a kind of clay with many interesting biological properties relevant to spinal cord injuries, including good biocompatibility (ability to avoid rejection by the body), safe biodegradation (breakdown and removal of the molecules after application), and excellent anti-inflammatory capability. LDH has already been widely explored in biomedical engineering with respect to immune response regulation, but mainly in the field of anti-tumor therapy.
“These properties made LDH a really promising candidate for the creation of a much more bene?cial microenvironment for spinal cord injury recovery,” says Rongrong Zhu of the
Department of Orthopedics of Tongji Hospital, first author of the study.
Under the leadership of Liming Cheng, corresponding author of the study, the research team transplanted the LDH into the injury site of mice, and found that the nanobiomaterial had signi?cantly accelerated neural stem cells migration, neural di?erentiation, activation of channels for neuron excitation, and induction of action potential (nerve impulse) activation. The mice were also found to enjoy significantly improved locomotive behavior compared to the control group of mice. In addition, when the LDH was combined with Neurotrophin-3 (NT3), a protein that encourages the growth and differentiation of new neurons, the mice enjoyed even better recovery effects than the LDH on its own. In essence, the NT3 boosts neuronal development while the LDH creates an environment where that development is allowed to thrive.
Then, via transcriptional profiling, or analysis of gene expression of thousands of genes at once, the researchers were able to identify how the LDH performs its assistance. They found that once LDH is attached to cell membranes, it provokes greater activation of the “transforming growth factor-β receptor 2” (TGFBR2) gene, decreasing production of the white blood cells that enhance inflammation and increasing production of the white blood cells that inhibit inflammation. Upon application of a chemical that inhibits TGFBR2, they found the beneficial effects were reversed.
The understanding of how LDH performs these effects should now allow the researchers to tweak the therapy to enhance its performance and to finally create a comprehensive therapeutic system for spinal cord injuries–combining these biomaterials with neurotrophic factors like NT3-that can be used in clinical application on people.
###
Media Contact
rongrong zhu
[email protected]
Related Journal Article
http://dx.




