UOC researchers have analysed 13 apps developed for the treatment and control of neglected tropical diseases, identifying the main weaknesses and evaluating possible improvements
Credit: UOC
A study performed by the Universitat Oberta de Catalunya (UOC) provided eight recommendations for improving the online technology to help with the treatment and diagnosis of neglected tropical diseases (NTDs). The analysis, presented in a recent open-access publication, was performed by UOC researchers Carme Carrion and Marta Aymerich from the eHealth Lab and Noemí Robles from the eHealth Center, together with José Antonio Ruiz Postigo from the World Health Organization and Oriol Solà de Morales from the Health Innovation Technology Transfer Foundation. In the study, the authors looked at the context of the existing apps and identified their weaknesses.
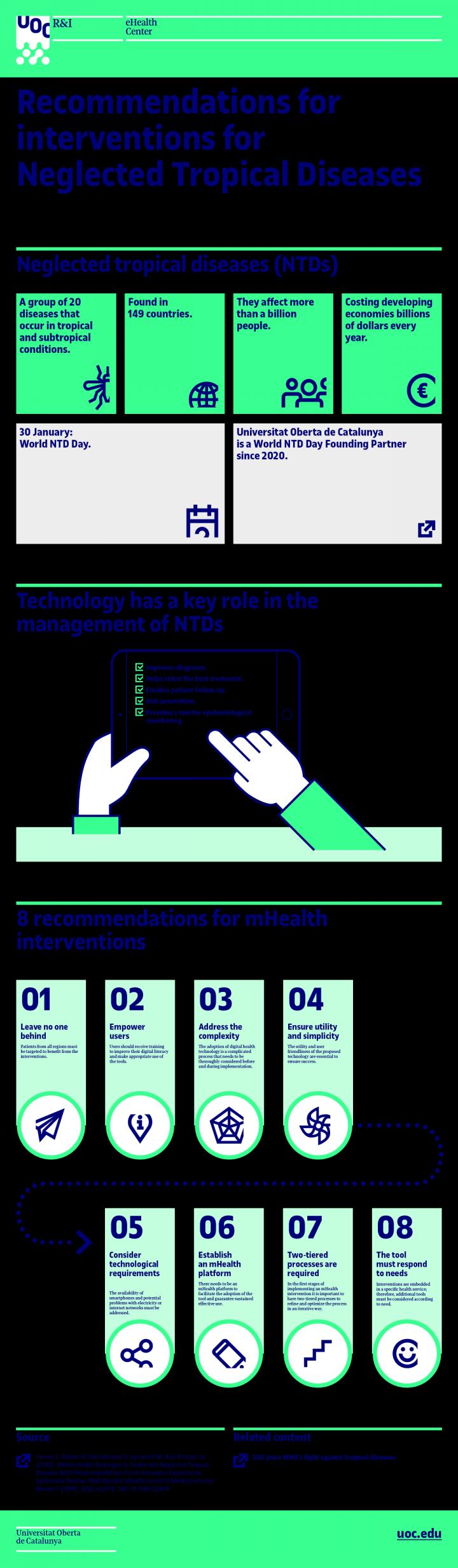
The recommendations, outlined in this infographic prepared by the UOC eHealth Center, are the result of analysing 13 apps out of a total of 133 candidates, and highlight both their weaknesses and their possibilities for improvement. The goal is to standardize and improve the apps developed for controlling and monitoring neglected tropical diseases of the skin, an even more neglected subgroup of NTDs.
Neglected tropical diseases affect more than a billion people and cause hundreds of thousands of deaths every year. In spite of this, most people still know very little about them. This is the second year that the World NTD Day has been held on 30 January.
More efficient, better uptake
The recommendations given by Carrion’s team in the form of a guide provide an initial base for improving the efficiency in the development and social uptake of apps designed for the control and treatment of NTDs. These recommendations are summarized in eight points:
Nobody should be left out: patients from all regions should be selected to benefit from the proposed interventions. This requires translating the tools into different languages. At the very least, into Portuguese and Spanish in the Americas; and English, French and Portuguese in Africa.
Users must have control: the interventions’ end users (health professionals and patients) must be given sufficient training to improve their digital literacy and make effective use of the tools that are provided.
Complexity must be adequately catered for: integrating e-health-related technology is a complicated process that should be considered in depth both before and during implementation.
Utility and simplicity must be there, and, what is more, they must be seen: health professionals, patients and healthy citizens must be able to understand the proposed technology’s utility and ease of use. In other words, it must be a facilitator, not a barrier.
The technological requirements must be considered from the beginning: the availability of adequate mobile devices, the potential problems with electricity supply or internet networks, and other technical issues must be considered as part of a comprehensive strategy with a specific objective.
A long-term m-health platform must be established: an m-health intervention’s success depends on the existence of a platform that makes it easier not only to implement the tool but also guarantees its sustained, effective use.
Split-level processes are required to improve: in the early stages of implementation of an m-health system, the processes must be divided into two levels in order, first, to refine the process and, then, to optimize it iteratively.
The tool must meet the stated needs: interventions are integrated in a specific health service; accordingly, additional tools should be considered as required.
One of the main challenges faced by this type of app, explained Carme Carrion, also affiliated with the UOC’s eHealth Center, is the digital divide, but not in its connotation as a knowledge problem: “The technological features are limited. You can’t design interventions that can only be used by a few people, because that widens the health gap and inequality,” said the expert. “You’ve got to look for simple, cheap solutions that leave no one behind, that can be taken to everyone, and not just these communities’ socioeconomic elites. That’s where the challenge is.”
E-health: an opportunity
“There are a series of problems in the countries where these diseases are endemic,” explained this expert in e-health solutions. “For example, access to mobile devices by the population, broad band, reliable internet connections, batteries […]. The number of existing apps related with tropical skin diseases is small. Compared with other, more general health apps, there are few apps available, even in Google Play or Apple Store. And the few that exist have virtually no scientific articles to back them,” she continued.
“WHO – who the UOC works with closely on increasing awareness of the NTDs – has been promoting m-health in these countries for more than 10 years, precisely because, in certain areas, in spite of the difficulties, it is much easier to communicate with a mobile phone and make video calls than to transport people physically.” However, “in order to do it well, we must have information that reviews the apps’ quality,” added the researcher, in order to improve their integration and the services that help combat this type of disease.
###
Media Contact
Sònia Armengou
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




