Researchers put forward a safe and efficient new stem cell therapy for regenerating cardiac function in pediatric patients
Credit: Okayama University Hospital
Dilated cardiomyopathy (DCM) is a condition caused by the weakening of the heart muscle, affecting the ventricles (chambers in the heart that push blood around the body as it contracts). If allowed to progress unchecked, DCM can lead to heart failure and death, especially in children. The only cure, at present, is a heart transplant, which comes with its own challenges: long waiting times to secure a suitable donor heart, the possibility of organ rejection, long hospitalizations and recovery times, among others.
In recent decades, stem cells have become the cornerstone of regenerative medicine, allowing medical professionals to treat damaged organs and reverse the course of several diseases that were previously deemed irrevocable. Scientists have turned to “cardiosphere-derived cells” (CDCs), a type of cardiac stem cells known to have beneficial effects in adults suffering from specific heart conditions. By developing (“differentiating”) into heart tissue, CDCs can reverse the damage inflicted by diseases. However, little is known about their safety and therapeutic benefit in children.
To address this problem, Professor Hidemasa Oh led an interdepartmental team of scientists at Okayama University, Japan, to launching the first steps to assess this therapy in children suffering from DCM. In a study published in Science Translational Medicine, the team not only showed the effectiveness of CDCs in replenishing damaged tissues in DCM but also revealed how this happens. Prof Oh explains the motivation, “I have been working on cardiac regeneration therapy since 2001. In this study, my team and I assessed the safety and efficacy of using CDCs to treat DCM in children .”
The first step of any trial when testing a new drug or therapy is to use animal models who react similarly to humans, which shows us whether the treatment is safe and has the intended effect. Thus, to begin with, the researchers tested this method in pigs, inducing cardiac symptoms similar to DCM and treating them with different doses of CDCs or a placebo. In those given the stem cell treatment, the scientists noticed quick improvements in cardiac function. The heart muscle thickened, allowing more blood to be pumped around the body. This effectively reversed the damage induced in the pigs’ hearts, an encouraging result leading them to progress to small, controlled human trials.
Their phase 1 trial involved five young patients suffering from DCM. The scientists now had a better idea of the suitable dose of CDCs to give their young patients, thanks to the pre-clinical trials in animals. One year after injection, the patients showed no sign of severe side effects from the treatment, but most importantly, there were encouraging signs of improved heart function. The authors are cautious: based on the small population size of their study, they cannot establish a strong conclusion. However, they are satisfied that CDC treatment appears sufficiently safe and effective to progress to a larger clinical trial. As Prof Oh explains, “We intend to move these results into a randomized phase 2 trial to obtain a pharmaceutical approval of this therapy in Japan .”
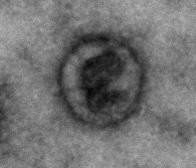
Another important finding was the mechanism through which CDCs actually lead to improved cardiac function. Indeed, their analyses revealed that transplanted cells secrete small vesicles called “exosomes,” which are enriched with proteins called “microRNAs” that initiate a whole cascade of molecular interactions. These microRNA-enriched exosomes have two effects. First, it blocks the damage-inducing cells from causing further harm to the heart tissue. Secondly, it induces the differentiation of stem cells into fully functioning cardiac cells (“cardiomyocytes”), starting the regenerative process. This generates hope that injecting these exosomes alone might be enough to reverse this type of heart damage in patients, bypassing the need for CDCs in the first place.
Looking back on their research, the scientists are hopeful that a phase 2 trial will confirm their suspicions, and what this could mean for future patients. Prospective transplant patients sometimes wait for years for a donor heart to become available. This type of therapy could allow them to live relatively normal lives, and even prevent the need for a transplant altogether for patients who have not yet reached such a critical stage.
###
Media Contact
Hidemasa Oh
[email protected]
Related Journal Article
http://dx.




