The widely used and well-tolerated drug commonly used to treat Parkinson’s disease may help significantly reduce the need for more costly, more invasive treatments, report investigators in The American Journal of Medicine
Credit: The American Journal of Medicine
Philadelphia, September 10, 2020 – Investigators have determined that treating patients with an advanced form of age-related macular degeneration (AMD) with levodopa, a safe and readily available drug commonly used to treat Parkinson’s disease, stabilized and improved their vision. It reduced the number of treatments necessary to maintain vision, and as such, will potentially reduce the burden of treating the disease, financially and otherwise. Their findings appear in the American Journal of Medicine, published by Elsevier.
More than 15 percent of the US population over the age of 70 has AMD, a common cause of blindness in developed nations. Neovascular AMD (nAMD) is characterized by the abnormal growth of new blood vessels, triggered by vascular endothelial growth factor (VEGF), which can cause fluid and blood to leak in the subretinal space of the eye. While nAMD represents only 10-15 percent of all AMD cases, it is responsible for 90 percent of the vision loss attributed to the disease. The standard treatment requires frequent injections of agents to block VEGF. While effective, the injections are expensive and painful.
Earlier research found that patients being treated with levodopa for movement disorders such as Parkinson’s disease were significantly less likely to develop any type of AMD. Lead investigator Robert W. Snyder, MD, PhD, Department of Biomedical Engineering, The University of Arizona, Tucson, and Snyder Biomedical Corporation, Tucson, AZ, USA, explained, “Levodopa has a receptor (GPR143) selectively expressed on pigmented cells. This receptor can be supportive of retinal health and survival, which led to the development of our hypothesis that it may prevent or treat AMD.”
The investigators developed two proof-of-concept studies to test whether levodopa improves visual acuity and the anatomical changes caused by nAMD. They also evaluated the safety and tolerability of the drug in treating nAMD and whether treatment reduced or delayed the need for anti-VEGF therapy.
In the first study, 20 patients newly diagnosed with nAMD who had never had VEGF treatment were given a small daily dose of levodopa for one month and were evaluated weekly by their referring retina specialist, who determined whether anti-VEGF treatment was needed. In the second part of the study, the patients who completed the first study and a second group of 14 patients who had received anti-VEGF treatment for at least three months before the study received escalating doses of levodopa to test the tolerance and efficacy of the drug. The patients continued to be evaluated monthly by their referring retina specialist.
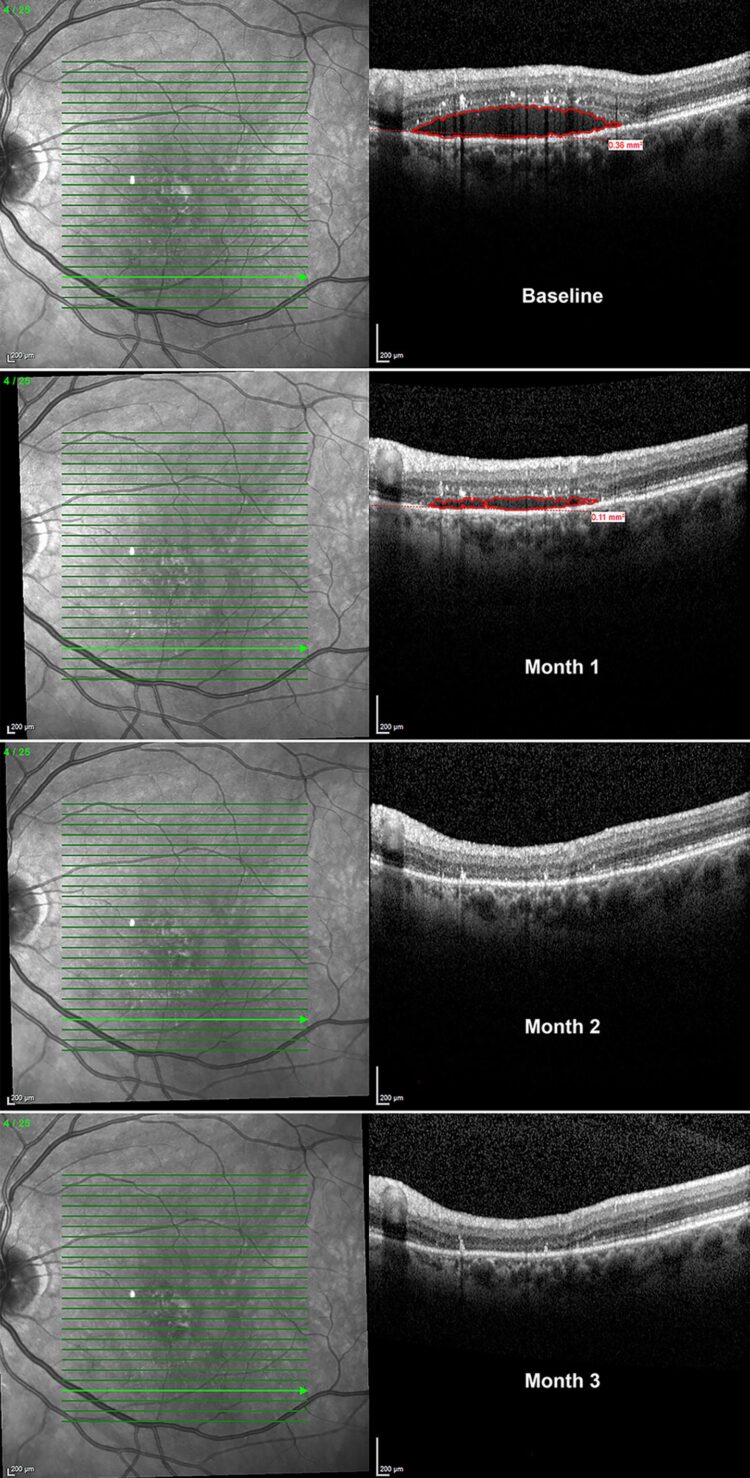
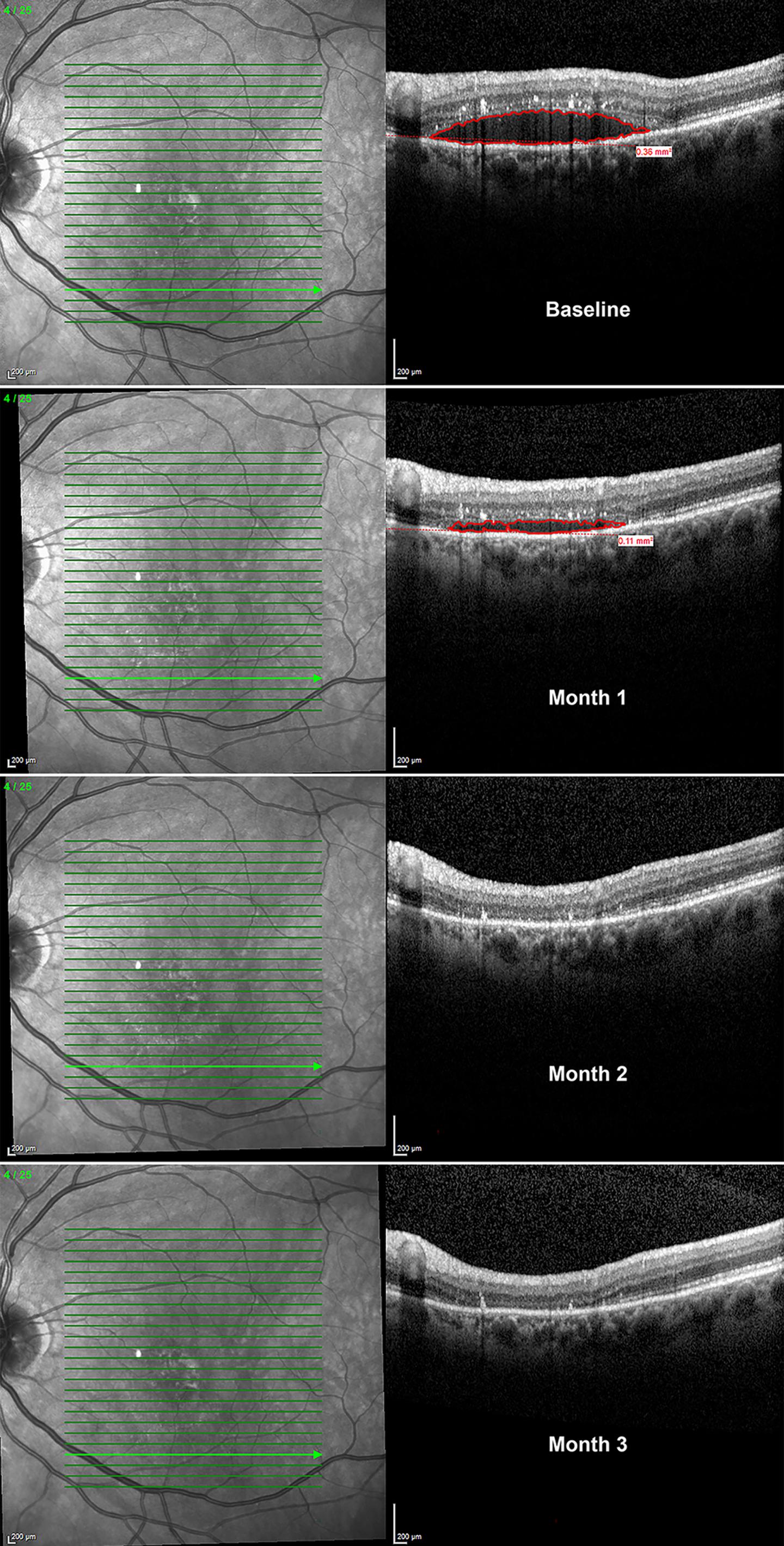
This trial demonstrated for the first time that levodopa is safe, well-tolerated, and delayed anti-VEGF injection therapy while improving visual outcomes. In the first month, retinal fluid decreased by 29 percent. After six months the decrease in retinal fluid was sustained and mean visual acuity improved enabling patients in the first and second group to read an additional line on the eye chart. This is the equivalent of improvement from 20/40 to 20/32. Side effects were limited.
The investigators noted that levodopa may be unlikely as a standalone treatment in patients with newly diagnosed nAMD since 11 of the patients did require anti-VEGF injections. However, they required fewer than the standard monthly treatments, and in the second group, monthly injections of anti-VEGF decreased by 52 percent.
According to Dr. Snyder, although this limited proof-of-concept study included a small sample size and limited patient diversity, its findings suggest efficacy and support the targeting of the GPR13 receptor with levodopa for the treatment of nAMD in future studies.
The concept had its genesis 20 years ago when Dr. Snyder began working with co-investigator Brian S. McKay, who had developed techniques to culture and examine retinal endothelial pigment cells. “We had a strong desire to make an impact in AMD, and I had a strong hunch that Dr. McKay could make a significant contribution,” Dr. Snyder said. “Although this is nowhere near completed, I am happy to say, 20 years later, we have all persevered, and I believe the GPR143/levodopa story will make a significant impact on our treatment and prevention of AMD.”
###
Media Contact
Jane Grochowski
[email protected]
Original Source
https:/
Related Journal Article
http://dx.