Credit: Cincinnati Children’s
When children are born with hypoplastic left heart syndrome (HLHS), they require a series of major surgical procedures to survive. But even with a repaired heart, as many as one in four children die from complications before age 25.
Now, a study published by a new faculty member at Cincinnati Children’s reports a potential therapeutic target that might promote heart cell regeneration even before birth.
Details were published online Aug. 17, 2020, in Cell Stem Cell.
ATLAS PROVIDES DEEP LOOK AT EARLY HEART DEVELOPMENT
Mingxia Gu, MD, PhD, formerly of Stanford University, joined the Center for Stem Cell & Organoid Medicine (CuSTOM) and the Division of Pulmonary Biology at Cincinnati Children’s earlier this year. She has been working for several years to find ways to prompt healing in damaged heart tissues.
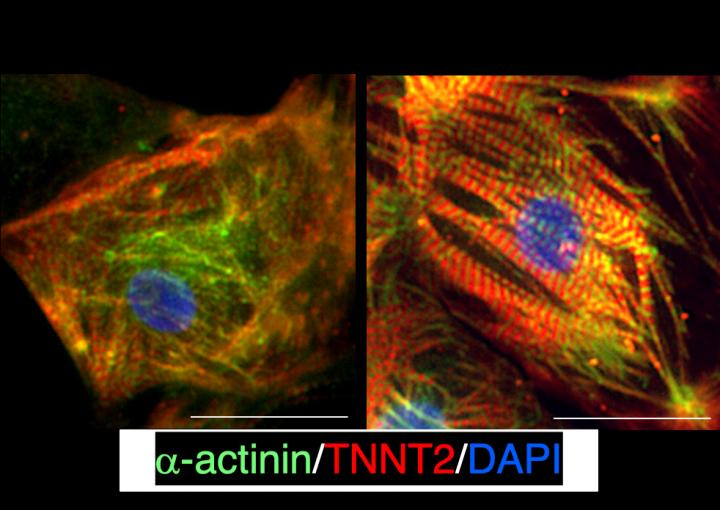
In this study, a team led by Gu and co-first authors Yifei Miao, PhD, and Lei Tian, PhD, used advanced single-cell transcriptomic analysis to develop a human heart “atlas” that tracks the full chorus of signals that endocardial cells send to each other as the heart develops during pregnancy.
Comparing this atlas of healthy heart development to data from lab-created induced pluripotent stem cells featuring HLHS defects revealed a collection of abnormalities in endocardial cells that disrupt healthy heart formation. Endocardial cells play several pivotal roles in heart development and disease. They can sense blood flow in the heart, interact with surrounding muscle cells, and give rise to key structures of the heart including atrioventricular valves and atrial and membranous ventricular septa.
Tracing HLHS-related disruptions to these cells represents a change in thinking compared to efforts that had been focused on myocardial cells, which form the beating muscle of the heart.
The hopeful news: the team found a potential therapeutic target that could be drugged to improve endocardial function, thus regenerating the cardiac valves, septum, and coronary vessels, and eventually increasing heart chamber size, which could reduce the need for multiple surgeries after birth.
WHAT IS HLHS?
Hypoplastic left heart syndrome results in infants born with a severely malformed cardiac left ventricle, the heart’s main pumping chamber. HLHS accounts for about 3% of all congenital heart defects, with a prevalence rate of 1 to 1.5 cases per 5,000 live births in the United States.
Treatment requires three surgeries to reroute blood flow so that the right ventricle can support all the work the heart must perform.
The unusual amount of pressure the repaired heart endures, plus other factors, can lead to heart failure that requires organ transplantation to treat.
For several years, scientists have tried various ways to use a person’s own stem cells to help damaged hearts heal. Most early efforts have had little success, especially for adults. In children, however, heart tissues continue to grow, which makes scientists more hopeful that stem cell therapies or other treatments might help improve daily health and life expectancy.
TREATMENT TARGET: FN1
Gu and colleagues found that the gene fibronectin (FN1) was significantly downregulated in HLHS endocardium. Various genetic abnormalities combined to impede FN1, leading to impaired valve formation and poor cardiomyocyte growth and maturation.
“Our discoveries provide a new facet to the pathogenesis of HLHS and an alternative angle for early intervention and cardiac regeneration in HLHS,” Gu says.
Given that fetal gene editing is not an option for human infants, more research is needed to determine whether a treatment to replace the missing functions of FN1 in HLHS can be developed for use after a child is born.
“The significance of this finding is that by discovering this gene’s role, we now have a target for future study,” Gu says.
###
Media Contact
Tim Bonfield
[email protected]
Related Journal Article
http://dx.




