Credit: CNIO
A team led by Massimo Squatrito, Head of the Seve Ballesteros Foundation Brain Tumour Group at the Spanish National Cancer Research Centre (CNIO), have made important findings of how some gliomas can acquire chemoresistance. Carried out together with the laboratory of Jiguang Wang from the Hong Kong University of Science and Technology (HKUST) and a clinical team led by Tao Jiang from Beijing Neurological Institute, and published in Nature Communications, the study provides also new clues on how to monitor the efficacy of therapy.
At present, the main, and virtually only, treatment for glioma – a very common type of tumour originating in the brain – is a combination of radiotherapy and the chemotherapy agent temozolomide. This type of treatment can improve patients’ survival rates by up to 30%. Similar to most of the chemotherapy drugs, temozolomide induces DNA damage in cancer cells. Gliomas can progress by repairing this damage through an enzyme encoded by the MGMT gene. In patients whose MGMT activity is blocked because of a modification of its promoter called ‘hypermethylation’, cancer cells cannot repair the temozolomide-induced damage and collapse.
Unfortunately, up to 40-50% of patients are intrinsically resistant to temozolomide. These patients express high levels of MGMT and the tumour continue growing under treatment. Now, the recent study carried out by the CNIO and the HKUST team shows that a subset of patients acquires a specific genetic alteration that can evade the combined therapy.
Control changes hands
“Translocation of the MGMT gene was observed in a group of patients,” says Massimo Squatrito. “These genomic rearrangements involve the fusion of MGMT with other genes, which means that MGMT is now regulated by the promoters it is fused with, that contributes to its overexpression. When this type of rearrangements take place, the temozolomide-induced DNA damage is very efficiently repaired and the glioma continues growing even under treatment.”
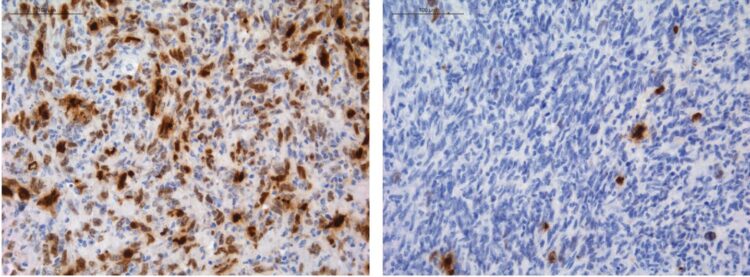
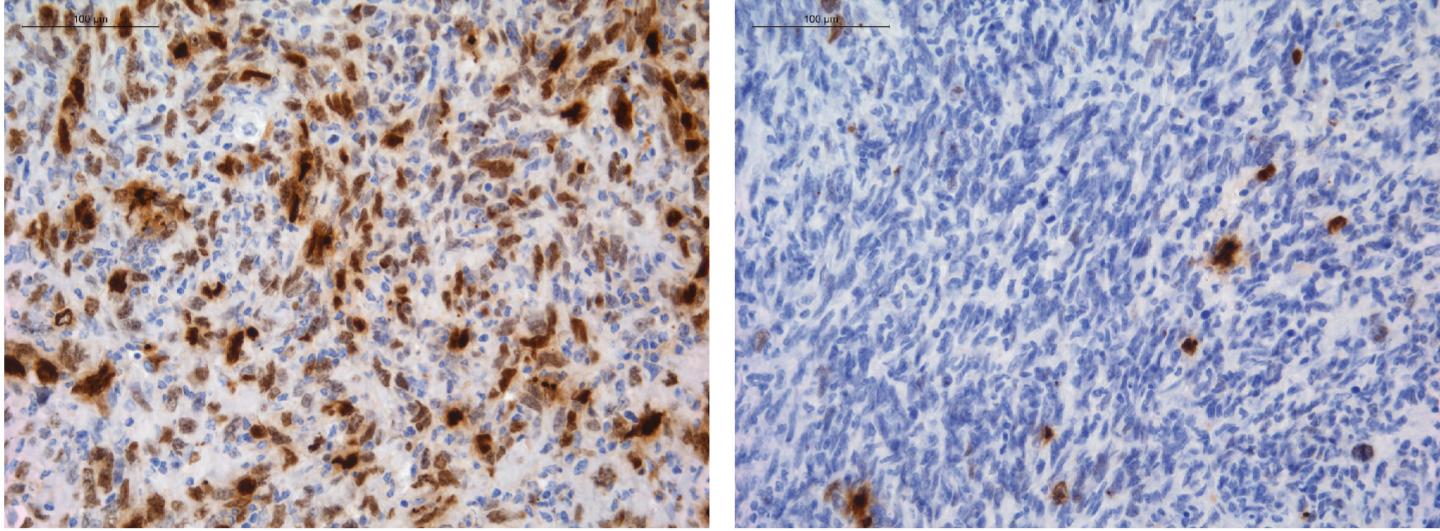
The team at the HKUST validated the presence of the genetic rearrangement in a subset of a large cohort of recurrent tumours, coming from different hospitals, mainly from Beijing Tiantan Hospital. Using the CRISPR-Cas9 genomic editing tool, the team at CNIO replicated some of these translocations in different cell and animal models and confirmed that they can confer resistance to temozolomide. “It appears that the translocations are not present in the original tumour, only in recurrent ones, that are, tumours that emerge after the original cancer is treated,” Squatrito says. “This indicates that the resistance may occur as a consequence to the treatment itself.”
The findings may lead to changes in the methods to monitor therapy efficacy: “Currently, the only known therapeutic biomarker in gliomas is the analysis of MGMT promoter status. When methylated, the MGMT gene is silenced and the patient is predicted to respond to temozolomide. The study shows this method is no longer valid when there has been a genetic translocation. The promoter might still be blocked, but the gene is being overactivated by other promoters and hence could contribute to tumour recurrence.”
Another relevant finding from animal models is that the MGMT translocations are present in exosomes -extracellular vesicles released by glioma cells into the bloodstream. “If this finding is validated in patients, it could become a useful tool for early resistance detection. A liquid biopsy, that is, a simple test using blood samples, could tell us when patients are developing resistance to temozolomide, and they could be advised to switch to other therapeutic options when they will become available.”
The next step will be identifying novel treatment intervention for the temozolomide resistant patients.
###
The study was funded by the National Institute of Health Carlos III of Spain, the Seve Ballesteros Foundation, the Spanish Association Against Cancer (AECC), the National Natural Science Foundation of China (NSFC), the Research Grants Council of Hong Kong, the Beijing Municipal Administration of Hospitals, the Beijing Nova Program and the Beijing Talents Foundation.
About The Hong Kong University of Science and Technology
The Hong Kong University of Science and Technology (HKUST) is a world-class research intensive university that focuses on science, technology and business as well as humanities and social science. HKUST offers an international campus, and a holistic and interdisciplinary pedagogy to nurture well-rounded graduates with global vision, a strong entrepreneurial spirit and innovative thinking. HKUST attained the highest proportion of internationally excellent research work in the Research Assessment Exercise 2014 of Hong Kong’s University Grants Committee, and is ranked as the world’s best young university in Times Higher Education’s Young University Rankings 2020. Its graduates were ranked 10th worldwide and top in Greater China in Global University Employability Survey 2019.
About the CNIO
The CNIO is a Spanish public institution dedicated to the research, diagnosis and treatment of cancer, and affiliated to the Carlos III Institute of Health (Ministry of Science, Innovation and Universities). It is one of the 10 leading cancer research centres in the world (Scimago Institutions Rankings World Report; Nature Index) and covers the entire R&D and Innovation spectrum, from basic research to the clinic, with a view to transferring the results quickly and efficiently to the National Health System and to the pharmaceutical and biotechnology market.
The CNIO has an Experimental Therapeutics Program that covers the initial stages of the development of drugs directed against the therapeutic targets its scientists are working on. Some of the CNIO’s compounds have been licensed to international pharmaceutical companies. In addition, the CNIO is actively involved in ‘open innovation’ programs of international pharmaceutical companies, which has resulted in an influx of more than 25 million euros into the CNIO in the past 6 years. Finally, three spin-off companies have emerged from the CNIO, which have also allowed patients to benefit from the centre’s developments. These data reflect the Institution’s commitment to innovation and technology transfer and illustrate the importance of public-private collaboration for the advancement in the diagnosis and treatment of disease.
Reference article: MGMT genomic rearrangements contribute to chemotherapy resistance in gliomas. Barbara Oldrini et al. (Nature Communications, 2020). DOI: 10.1038/s41467-020-17717-0
Media Contact
Vanessa Pombo
[email protected]
Original Source
https:/
Related Journal Article
http://dx.