Rice, Texas Heart Institute scientists model how synthetic gels can tune body’s inflammatory response
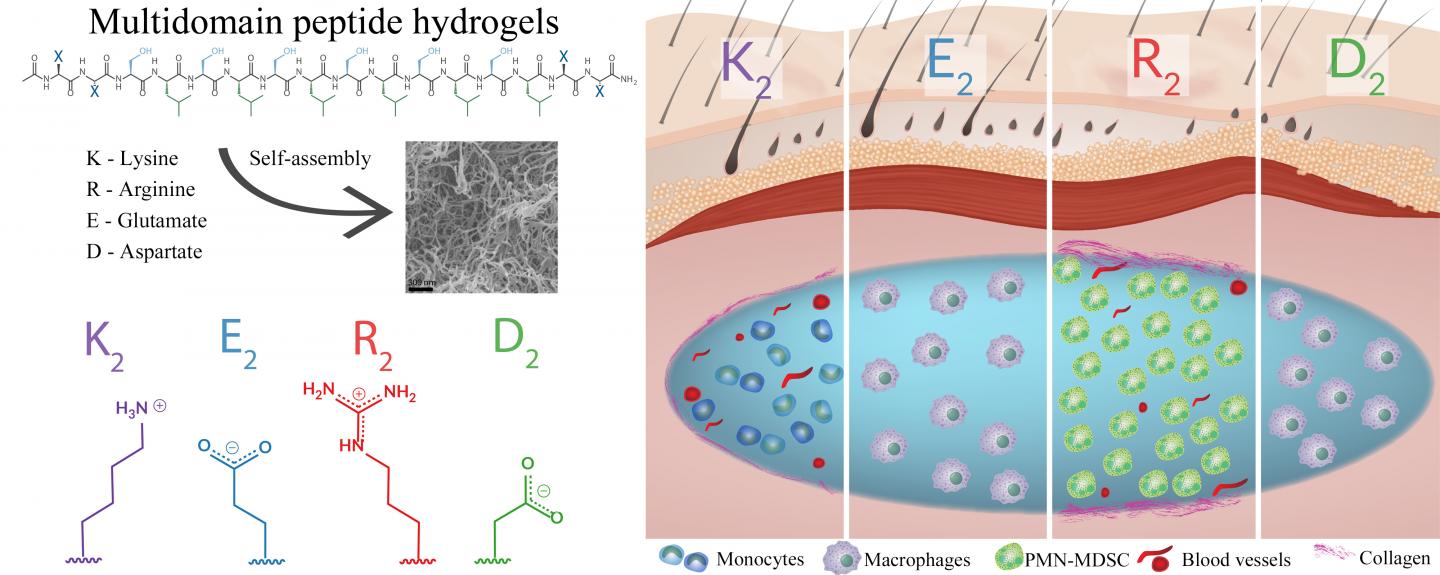
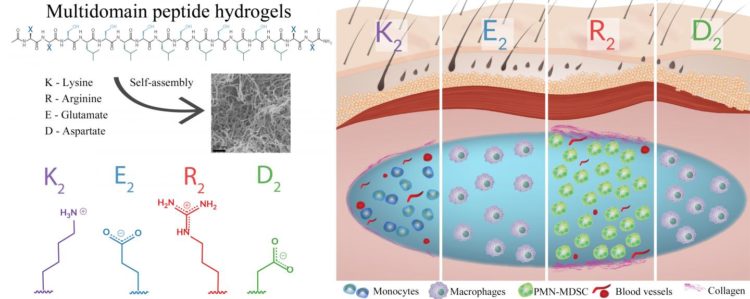
Credit: Illustration by Tania Lopez-Silva/Rice University
HOUSTON – (Dec. 16, 2019) – Hydrogels for healing, synthesized from the molecules up by Rice University bioengineers, are a few steps closer to the clinic.
Rice researchers and collaborators at Texas Heart Institute (THI) have established a baseline set of injectable hydrogels that promise to help heal wounds, deliver drugs and treat cancer. Critically, they’ve analyzed how the chemically distinct hydrogels provoke the body’s inflammatory response — or not.
Hydrogels developed at Rice are designed to be injectable and create a mimic of cellular scaffolds in a desired location. They serve as placeholders while the body naturally feeds new blood vessels and cells into the scaffold, which degrades over time to leave natural tissue in its place. Hydrogels can also carry chemical or biological prompts that determine the scaffold’s structure or affinity to the surrounding tissue.
The study led by chemist and bioengineer Jeffrey Hartgerink and graduate student Tania Lopez-Silva at Rice and Darren Woodside, vice president for research and director of the flow cytometry and imaging core at THI, demonstrates it should be possible to tune multidomain peptide hydrogels to produce appropriate inflammatory response for what they’re treating.
The research appears in Biomaterials.
“We’ve been working on peptide-based hydrogels for a number of years and have produced about 100 different types,” Hartgerink said. “In this paper, we wanted to back up a bit and understand some of the fundamental ways in which they modify biological environments.”
The researchers wanted to know specifically how synthetic hydrogels influence the environment’s inflammatory response. The two-year study offered the first opportunity to test a variety of biocompatible hydrogels for the levels of inflammatory response they trigger.
“Usually, we think of inflammation as bad,” Hartgerink said. “That’s because inflammation is sometimes associated with pain, and nobody likes pain. But the inflammatory response is also extremely important for wound healing and in clearing infection.
“We don’t want zero inflammation; we want appropriate inflammation,” he said. “If we want to heal wounds, inflammation is good because it starts the process of rebuilding vasculature. It recruits all kinds of cells that are regenerative to that site.”
The labs tested four basic hydrogel types — two with positive charge and two negative — to see what kind of inflammation they would trigger. They discovered that positively charged hydrogels triggered a much stronger inflammatory response than negatively charged ones.
“Among the positive materials, depending on the chemistry generating that charge, we can either generate a strong or a moderate inflammatory response,” Hartgerink said. “If you’re going for wound-healing, you really want a moderate response, and we saw that in one of the four materials.
“But if you want to go for a cancer treatment, the higher inflammatory response might be more effective,” he said. “For something like drug delivery, where inflammation is not helpful, one of the negatively charged materials might be better.
“Basically, we’re laying the groundwork to understand how to develop materials around the inflammatory responses these materials provoke. That will give us our best chance of success.”
The THI team helped analyze the cellular response to the hydrogels through multidimensional flow cytometry.
“The results of this work lay the groundwork for specifically tailoring delivery of a therapeutic by a delivery vehicle that is functionally relevant and predictable,” Woodside said. “Aside from delivering drugs, these hydrogels are also compatible with a variety of cell types.
“One of the problems with stem cell therapies at present is that adoptively transferred cells don’t necessarily stay in high numbers at the site of injection,” he said. “Mixing these relatively inert, negatively charged hydrogels with stem cells before injection may overcome this limitation.”
Hartgerink said the work is foundational, rather than geared toward a specific application, but is important to the long-term goal of bringing synthetic hydrogels to the clinic. “We have been speculating about a lot of the things we think are good and true about this material, and we now have more of a sound mechanistic understanding of why they are, in fact, true,” Hartgerink said.
###
Co-authors of the paper are Rice graduate student David Leach and alumnus I-Chi Li and THI researcher Alon Azares.
The National Institutes of Health, the Welch Foundation, the Mexican National Council for Science and Technology, the National Science Foundation and a Stauffer-Rothrock Fellowship supported the research.
Read the abstract at https:/
This news release can be found online at https:/
Follow Rice News and Media Relations via Twitter @RiceUNews.
Related materials:
Slow-release hydrogel aids immunotherapy for cancer: http://news.
Hydrogel may help diabetic ulcers: http://news.
Smart scaffolding aims to rebuild tissue from the inside: http://news.
Hydrogels deliver on blood-vessel growth: http://news.
‘Sticky’ ends start synthetic collagen growth: http://news.
Hartgerink Research Group: http://www.
Darren Woodside: https:/
Rice Department of Chemistry: http://chemistry.
Rice Department of Bioengineering: http://bioe.
Images for download:
https:/
An illustration shows how effective a selection of custom-designed peptide hydrogels are in controlling inflammation. The gels developed at Rice University serve as scaffolds for new tissue and show promise for treating wounds and cancer and for delivering drugs. The hydrogels are designed to dissolve in the body as they are replaced by natural, functional tissue. (Illustration by Tania Lopez-Silva/Rice University)
https:/
Researchers at Rice University and Texas Heart institutes tested a sampling of synthetic, biocompatible hydrogels to see how tuning them influences the body’s inflammatory response. The hydrogels are being developed to help heal wounds, deliver drugs and treat cancer. (Credit: Rice University/Texas Heart Institute)
The Texas Heart Institute (THI), founded by world-renowned cardiovascular surgeon Dr. Denton A. Cooley in 1962, is a nonprofit organization dedicated to reducing the devastating toll of cardiovascular disease through innovative and progressive programs in research, education and improved patient care. More information about THI (@Texas_Heart) is available at http://www.
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation’s top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 3,962 undergraduates and 3,027 graduate students, Rice’s undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for lots of race/class interaction and No. 4 for quality of life by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger’s Personal Finance.
Contacts:
AT RICE:
Jeff Falk
713-348-6775
[email protected]
Mike Williams
713-348-6728
[email protected]
AT TEXAS HEART INSTITUTE:
Keri Sprung
832-355-9240
[email protected]
Media Contact
Mike Williams
[email protected]
713-348-6728
Original Source
https:/
Related Journal Article
http://dx.