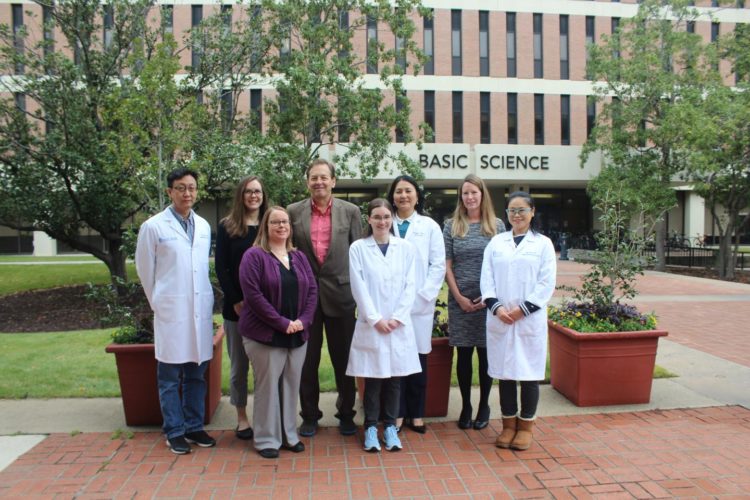
First NIH-funded clinical trial in the US using umbilical cord derived mesenchymal stem cells for the treatment of patients with new onset type 1 diabetes
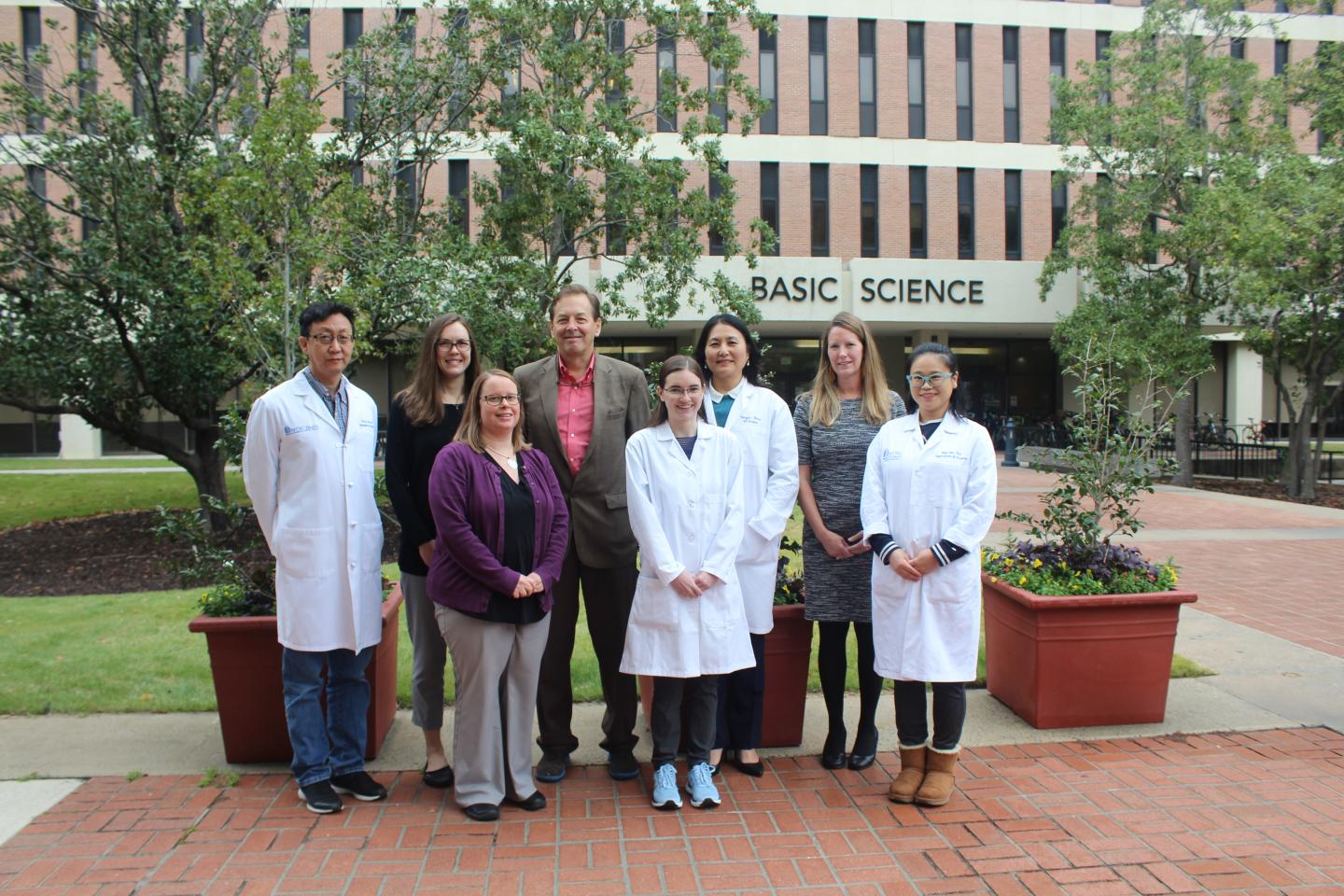
Credit: Medical University of South Carolina
Type 1 diabetes (T1D) is a chronic condition in which the body’s own immune system attacks and destroys beta cells in the pancreas. Once the beta cells are destroyed, the pancreas can no longer produce insulin. Currently, there is no cure for T1D and treatment focuses on managing blood sugar levels.
Researchers at MUSC, including Hongjun Wang, Ph.D., tenured professor in the Department of Surgery, hope to offer patients a better alternative.Wang joined MUSC eight years ago, believing the excellence in islet cell transplantation, a clean cell facility, and a focus on population health provided the perfect opportunity for her to conduct research that she hopes will lead to a cure for patients with T1D.
“I am very grateful Dr. Baliga recruited me eight years ago,” said Wang. “MUSC provides the resources to build on what I learned at Harvard under my mentor, Fritz Bach, M.D., a brilliant transplant immunologist, and apply it to my work in islet cell transplantation and T1D.”She adds the opportunity to work collaboratively with other investigators who are also passionate about translating the basic science to solutions for patients suffering from diabetes is important.
“I am very lucky to work with such passionate people like Charlie Strange, M.D., Deborah Bowlby, M.D. and Gary Gilkeson, M.D., among others,” said Wang. Strange serves as the co-investigator of a $2M National Institutes of Health grant to explore novel treatments for patients with T1D using animal models, combining Wang’s expertise in islet biology and immunology and Strange’s expertise in AAT biology and genomics. This grant is part of a series of NIH funded grants in the Wang Lab, one of the most highly funded labs in the Department of Surgery. Currently the Wang Lab has four NIH funded grants running concurrently as well as a Veterans Affairs Administration Merit Award and private funding.
“The beauty of our lab at MUSC is the ability to do translational research,” said Wang. “We can study the mechanisms of the disease on the bench and then have the ability to move to the bedside in a clinical trial.” This fall, their effort in the lab moved the science forward and they are now enrolling patients in a clinical trial to study mesenchymal stem cells (MSCs) from umbilical cord (UC-MSCs) as a possible therapeutic for patients with early onset T1D. The use of mesenchymal stem cells (MSCs) as a therapeutic tool to reduce progression of T1D represents a promising new intervention.
A pilot clinical trial in Sweden showed that a single infusion of autologous bone marrow derived MSCs preserved insulin secretion in adult patients with new onset T1D.
“MSCs derived from umbilical cord (UC-MSCs) show greater cell yield, a less invasive harvesting procedure with associated reduced morbidity, and stronger immunosuppressive and regenerative potential and are a popular source for cell therapy,” said Wang. “Based on the above principles, MUSC is embarking on a randomized, double blind, placebo controlled single center clinical trial to determine the efficacy of UC-MSC therapy in patients with new onset T1D.”
Contingent on enrollment of six newly diagnosed T1D adult patients, the NIH funded trial will be $3.5M over a five year period.
The clinical trial hypothesis is that systemic administration of MSCs freshly expanded ex vivo reduces progression of diabetes and preserves insulin secretion through restoring normal function of the immune system and preservation/improvement of pancreatic cells in patients with T1D.
###
To learn more about the clinical trial, visit http://www.
Media Contact
Heather Woolwine
[email protected]
843-792-7669
Original Source
https:/