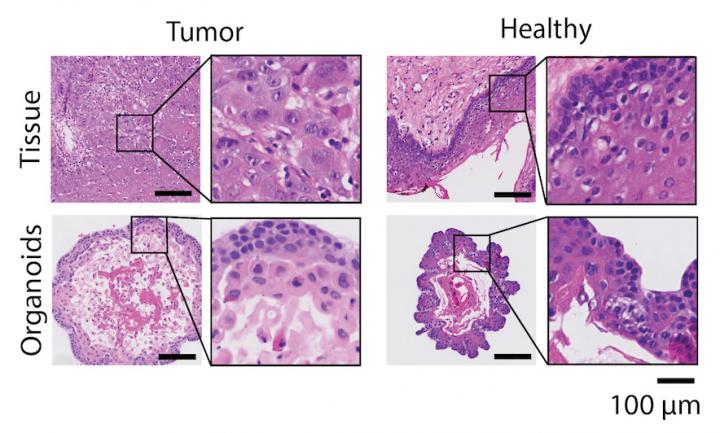
Credit: Else Driehuis, © Hubrecht Institute
Head and neck cancer is an aggressive type of cancer that often grows back, despite patients undergoing harsh treatments. Researchers of the Hubrecht Institute (KNAW) and UMC Utrecht succeeded in growing mini-tumors (or organoids) of head and neck cancers, that can be kept alive in the petri-dish for a long time. Else Driehuis, researcher at the Hubrecht Institute: “These mini-tumors can be used to better understand this complex disease. Moreover, organoids allow us to test both novel and existing therapies in the lab, without burdening the patient.”
Head and neck cancer is amongst the ten most prevalent cancers in the world. In the Netherlands, more than 3000 people are diagnosed with this disease every year. Despite heavy treatments that include surgery, radiotherapy and chemotherapy, this aggressive type of cancer grows back within two years in 40 to 60% of the patients. This results in problems with speaking and swallowing and can have large consequences for the physical appearance of the patient. “The treatment of head and neck cancer is harsh”, according to medical oncologist Lot Devriese (UMC Utrecht). Often, a combination of therapies is required to treat the disease and this can result in serious side effects. Therefore, there is an urgent need to make treatments more effective and decrease side effects.”
Surgery
Researchers working in the group of Hans Clevers (Hubrecht Institute) and doctors and researchers from the UMC Utrecht have now shown that organoids can be grown from so-called head and neck squamous cell carcinomas (HNSCC). These mini-organs are derived from patient-material, for example obtained from the tumor mass removed during surgery. Tumor-organoids of thirty patients diagnosed with head and neck cancer have been kept in culture for over a year. “This is the first time that researchers have been successful in growing organoids derived from head and neck cancer on this scale” says pathologist Stefan Willems (UMC Utrecht). “This technique allows us to multiply the tumor cells of a patient in the lab and will contribute to our understanding of head and neck cancer.”
Radiotherapy
After growing the mini-tumors, they were exposed to chemotherapies that are currently given to patients with head and neck cancer. Since radiotherapy is also a common component of the treatment of these patients, the organoids were also exposed to radiotherapy. For seven patients their response to radiotherapy was known. Upon exposure to this therapy, the organoids derived from these patients behaved in the same way as the tumors in these patients did. “We have now started a study in which we will include more patients, to see if organoids can indeed predict the patients response to therapy”, says Else Driehuis (Hubrecht Institute).” At the moment, many patients are exposed to harsh chemotherapeutics, whereas some of them in hindsight did not benefit from this therapy. In the lab, we can test many different drugs at the same time to see how the tumor-organoids of the patient respond to them. Potentially, such tests can help us to choose the right therapy for each individual patient.”
Predicting patient response
The researchers also exposed the mini-tumors to a range of novel drugs, so-called ‘targeted therapies’. As the name implies, these drugs have a very targeted effect and therefore cause less severe side effects than conventional chemotherapies. The downside: they only work for a subset of patients that carry specific alterations in the DNA of their tumor. “For some of these drugs, it has proven difficult to predict which patients will benefit from the treatment. Unfortunately, this has limited the success of these promising therapies so far” says Driehuis. “In our study, we observed that each of the drugs we tested was effective in the organoids of at least one patient. More research will tell us if the tumor-organoids can also predict the patient response for these therapies.”
###
Publication
Oral mucosal organoids as a potential platfom for personalized cancer therapy. Else Driehuis, Sigrid Kolders, Sacha Spelier, Kadi Lõhmussaar, Stefan M. Willems, Lot A. Devriese, Remco de Bree, Emma J. de Ruiter, Jeroen Korving, Harry Begthel, Johan H. van Es, Veerle Geurts, Gui-Wei He, Richard H. van, Jaarsveld, Rurika Oka, Mauro J. Muraro, Judith Vivié, Maurice M.J.M. Zandvliet, Antoni P.A. Hendrickx, Nino Iakobachvili, Priya Sridevi, Onno Kranenburg, Ruben van Boxtel, Geert Kops, David A. Tuveson, Peter J. Peters, Alexander van Oudenaarden and Hans Clevers. Cancer Discovery 2019.
Hans Clevers is group leader at the Hubrecht Institute, professor of Molecular Genetics at the UMC Utrecht and Utrecht University, Research Director of the Princess Máxima Center for Pediatric Oncology and Oncode Investigator.
About the Hubrecht Institute
The Hubrecht Institute is a research institute focused on developmental and stem cell biology. It encompasses 24 research groups that perform fundamental and multidisciplinary research, both in healthy systems and disease models. The Hubrecht Institute is a research institute of the Royal Netherlands Academy of Arts and Sciences (KNAW), situated on the Utrecht Science Park. Since 2008, the institute is affiliated with the UMC Utrecht, advancing the translation of research to the clinic. The Hubrecht Institute has a partnership with the European Molecular Biology Laboratory (EMBL). For more information, visit http://www.
Note for the press
For more information, please contact Melanie Fremery, the communications officer of the Hubrecht Institute: [email protected] or 0031658911260 (between during 9:00AM and 6:00PM Dutch time).
Media Contact
Melanie Fremery
[email protected]
Original Source
http://cancerdiscovery.
Related Journal Article
http://dx.




