Credit: Sandra Gabelli
The cell membrane is a fatty layer that forms a border between the inside of the cell, its various structures and the outside world. Embedded in these layers of fat, like tiles in a mosaic, are proteins that allow the cell to communicate with its neighbors, remove waste, regulate its composition and create energy.
So-called membrane channels are one type of such proteins. These channels are large proteins embedded in the cell membrane that create a gated path through the cell’s outside border. These channels are often specific to one type of molecule, allowing the cells to have fine control over what moves in and out. This tip sheet includes summaries of new research on these intriguing proteins and their functions within the cell.
Differences Between Skeletal and Heart Muscle Ion Channel Lends Insight into Inherited Heart Disease
Published April 3 in Nature Communications
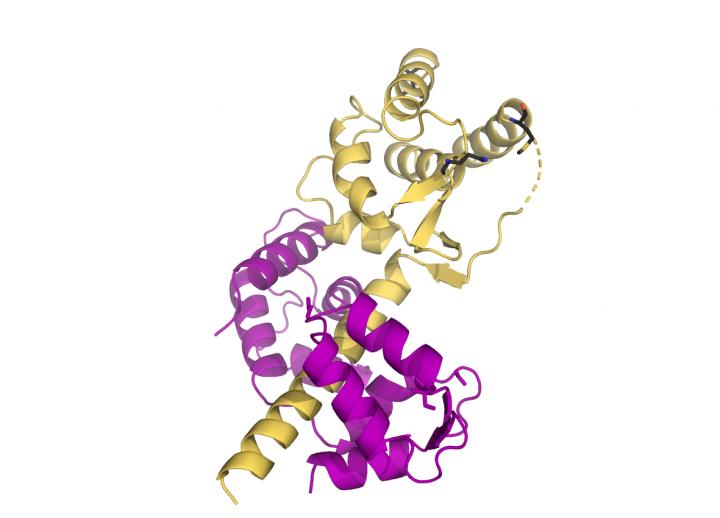
Johns Hopkins Medicine researchers recently found a key structural differences in channels that regulate how and when heart and skeletal muscles contract. Identifying the differences between the two, say researchers, provides scientists with new potential drug targets to treat inherited heart disease.
Muscle function depends on a voltage gradient between the inside of the cell and the outside — positive charges build up outside of the cell and negative charges remain inside. When signaled to contract, the cells open channels through their cell membranes, allowing positively charged molecules to flow in.
The researchers found that skeletal muscles can be regulated by a calcium-carrying protein called calmodulin. In the presence of calcium, this protein connects to the sodium ion channel and dampens its response, slowing the rate at which it transports sodium ions into the cell. The researchers say this may allow the cells to finely tune the strength of their contractions. On the other hand, the sodium ion channels in heart muscle cells do not change their sodium conductance in response to calmodulin.
The researchers suspect that genetic mutations could cause the sodium ion channel in heart muscle cells to behave more like the skeletal muscle channel, causing the cells to respond to calmodulin when they should not. This, say the researchers, could contribute to inherited arrhythmias, such as cold-aggravated myotonia and potassium-aggravated myotonia. There are currently no treatments addressing the cause of these diseases, and identifying the differences between the sodium ion channels in these two muscle types provides an opening for targeted drug development.
Authors of this study include Jesse Yoder, Federica Farinelli, Lakshmi Srinivasan, Sophie Shoemaker, Sandra Gabelli and Mario Amzel of the Johns Hopkins University School of Medicine; Manu Ben-Johny of Columbia University; and Gordon Tomaselli of the Albert Einstein College of Medicine.
This work was funded by the National Heart, Lung and Blood Institute (HL128743).
Prevalent Membrane Molecule Is Vital to Produce Energy for the Cell
Published March 29 in Nature Communications
Membranes are made up of a mix fatty molecules known as lipids that create a border between the outside and the inside of cellular structures. Mitochondria, for example, have two membranes that separate them from the rest of the cell.
The mitochondrial membranes hold important structures that allow the mitochondria to produce energy for the cell as well as essential molecules for the cell’s well-being. In fact, mitochondria create the second most abundant lipid in cellular membranes, called phosphatidylethanolamine. Though there are other places in the cell that create phosphatidylethanolamine, past studies showed that the lipids made in the mitochondria are special. When mitochondria stop creating phosphatidylethanolamine, cells shut down.
To investigate why, Johns Hopkins Medicine researchers took a closer look at phosphatidylethanolamine’s function inside the mitochondria of yeast. They found that if the mitochondria’s ability to produce phosphatidylethanolamine was turned off, the mitochondria’s energy factories did not work properly, even though the lipid was present in the rest of the cell.
The researchers suspect that this is because the mitochondrial membrane only allows small amounts phosphatidylethanolamine to be transported back into the mitochondria. That is why, they say, it is important that the lipid is locally sourced. It ensures that there is enough phosphatidylethanolamine to power the mitochondria’s energy factories.
Authors of this study include Elizabeth Calzada, Erica Avery, Pingdewinde Sam, J. Michael McCaffery and Steven Claypool of the Johns Hopkins University School of Medicine; Arnab Modak and Nathan Alder of the University of Connecticut; and Chunyan Wang and Xianlin Han of the University of Texas Health Science Center.
Funding for this research was provided by the National Institute of General Medical Sciences (R01GM111548, R01GM111548-03S1, T32GM007445, R01GM113092) and the National Science Foundation Graduate Research Fellowship (DGE1746891).
Helper Cells May Cause More Harm than Good in Brain Injury
Published April 11 in Neuron
Johns Hopkins Medicine researchers have found that cells previously thought to only play a supportive role in the central nervous system may be key contributors to nerve damage in cases of brain injury. The researchers found that these supportive cells, known as astrocytes, have channels through the cell membrane that regulate messages in the brain. The discovery of this channel on astrocytes unveils a new target for therapies for brain-damaging diseases such as stroke and traumatic brain injury.
Injury causes brain cells to swell, which can further damage the surrounding tissue. To relieve the pressure, cells will open channels and spray out their contents. One such gate is the volume-regulated anion channel (VRAC). This newly-discovered channel releases the important neurotransmitter glutamate.
Glutamate plays a vital role in creating and strengthening connections between signaling neurons. However, glutamate must be tightly regulated as high levels can be toxic to neurons. The researchers suspect that in brain injury, such as stroke, the astrocytes can respond by opening VRAC. This would flood the surrounding area with glutamate, harming neighboring neurons.
Authors of this study include Junhua Yang, Maria del Carmen Vitery, Jianan Chen, James Osei-Owusu, Jianchen Chu and Zhaozhu Qiu of the Johns Hopkins University School of Medicine.
Funding for this research was provided by the National Institute of General Medical Sciences (R35GM124824) and the American Heart Association.
To follow up on these stories, please contact Rachel Butch [email protected].
###
Media Contact
Rachel Butch
[email protected]




