NIH study finds new cell composition may lead to less effective future response
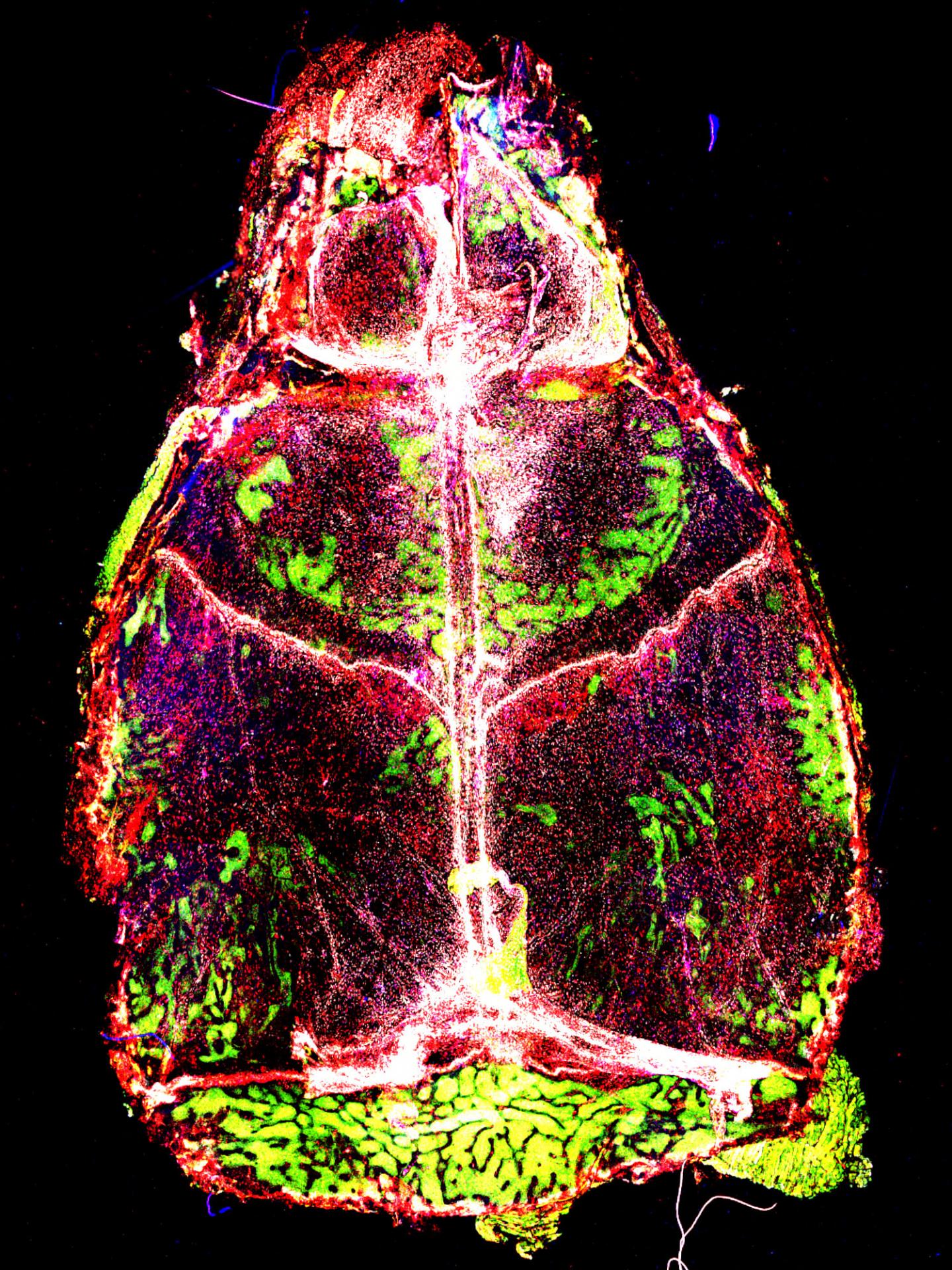
Credit: Image courtesy of the McGavern Lab, NINDS.
Meningitis, a group of serious diseases which infect the brain’s lining, leaves its mark and can affect the body’s ability to fight such infections in the future. According to a new study published in Nature Immunology, infections can have long-lasting effects on a population of meningeal immune cells, replacing them with cells from outside the meninges that then change and become less likely to recognize and ward off future attacks. The research was supported by the National Institute of Neurological Disorders and Stroke (NINDS), part of the National Institutes of Health.
“After an infection, the immune cell landscape in the brain lining changes. Brain lining immune cells that normally protect the brain from foreign invaders die and are replaced by cells from elsewhere in the body. These new cells are altered in a way that affects how they respond to subsequent challenges and new infections,” said Dorian McGavern, Ph.D., NINDS scientist and senior author of the study.
Using real time imaging, Dr. McGavern and his colleagues took a detailed look at mouse meningeal macrophages, which are immune cells that live in the meninges, the protective layers covering the brain and spinal cord. One group of these macrophages is found along blood vessels in the dura mater (the outermost layer of the meninges) and helps catch pathogens from the blood before they reach brain tissue. Blood vessels in the dura mater are relatively open compared to the tightly sealed vessels found in other brain regions, and macrophages in the dura mater often serve as the first line of defense against harmful blood-borne agents.
Dr. McGavern and his team observed that during normal conditions, meningeal macrophages were on constant alert against threats, continually extending their thin arms and surveying their environment.
They next watched how macrophages changed after infection by lymphocytic choriomeningitis virus (LCMV), which targets the meninges, causing viral meningitis. Within two days of the infection, levels of antiviral cytokines, part of the immune response to viruses, increased in the meninges. After four days, one-third of meningeal macrophages were infected, and showed activity in many genes involved in fighting viruses.
Dr. McGavern and his colleagues then investigated the long-term effects of this infection, after the virus was cleared and the meningitis had subsided. Within a week, most of the infected macrophages had died and were removed from the area by immune cells, leaving a depleted stock of meningeal macrophages. This supply was refilled by monocytes, immune cells recruited from the blood.
Some of these monocytes eventually turned into macrophages but had different properties from the original cells. The team discovered that the new macrophages were missing a specific receptor that detects bacteria, making them less effective at responding to future infections.
The new macrophages also had lower levels of another receptor that recognizes the brain chemical acetylcholine, which normally dulls inflammation in meningeal macrophages. Consequently, the new macrophages were less responsive to this signal and had trouble quieting an infection-induced inflammatory response. These results indicate that infections in the brain can have lasting effects, long after the virus leaves the system.
“These findings suggest that in addition to identifying the type of infection, it may also be important to know if it is coming on the heels of an earlier bug because that may affect how the system responds,” said Dr. McGavern. “Getting a virus out of the brain does not necessarily mean that everything goes back to normal.”
Further studies are needed to learn about additional functions of meningeal macrophages and how these cells respond to other types of viruses and bacteria.
###
This work was supported by the NIH Intramural Research Program.
For more information:
http://www.
neuroscience.nih.gov/ninds/Home.aspx
Image caption: Cells on the lookout. Meningeal macrophages (shown in white, red, and blue) are on constant alert against potential threats to brain tissue. Image courtesy of the McGavern Lab, NINDS.
References:
Rua R et al. Infection drives long-term meningeal engraftment by inflammatory monocytes that impair central nervous system immunity. Nature Immunology.
The NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.
Media Contact
Barbara McMakin
[email protected]
Related Journal Article
http://dx.



