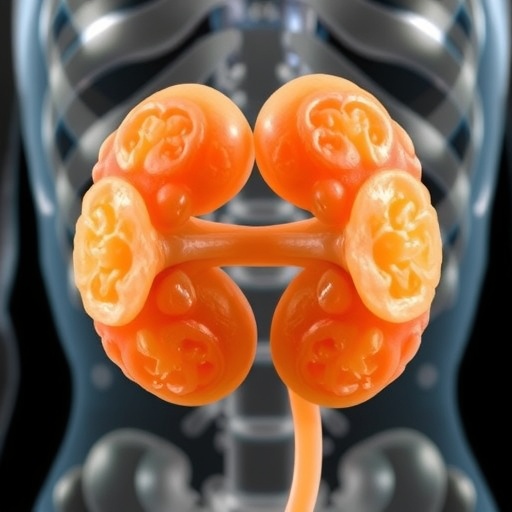
In a groundbreaking advancement in cancer research, scientists at Tsinghua University have pioneered a novel technique to culture kidney tumors in laboratory settings directly derived from patient cells. This cutting-edge approach, detailed in a recent study published in the prestigious journal Biofabrication, leverages sophisticated 3D bioprinting technology to fabricate renal cell carcinoma (RCC) organoids that retain the distinct biological hallmarks of the original tumors. By integrating multiple cellular components, including tumor cells and vascular-like structures, the research team has generated a dynamic cellular microenvironment that closely mirrors in vivo conditions, offering unprecedented accuracy for therapeutic testing and cancer biology exploration.
Traditional models used to study RCC and evaluate treatment efficacy have long suffered from significant drawbacks. Conventional two-dimensional cell cultures and animal models often fail to replicate the intricate heterogeneity and microarchitecture of human tumors, which critically influences therapy responses and disease progression. Tumors are not homogenous masses but complex ecosystems composed of varied cell populations and extracellular matrix interactions, factors that contribute to intratumoral diversity and adaptive resistance mechanisms. This complexity underlies the high variability in patient responses to chemotherapy and targeted drugs, rendering generalized treatment protocols often ineffective.
The innovative 3D bioprinting methodology developed by the Tsinghua team builds upon advances in biomaterial science, tissue engineering, and cellular biology. Utilizing patient-derived tumor cells as bioinks, the researchers were able to engineer multi-cellular constructs that incorporate endothelial-like networks, simulating the blood vessels that nourish tumors in the human body. This replication of vasculature is crucial, as it influences tumor metabolism, growth, and the delivery of therapeutic agents, factors typically absent or poorly modeled in traditional systems. These organoids thus serve as robust, physiologically relevant platforms that reflect tumor heterogeneity and microenvironmental dynamics with exceptional fidelity.
.adsslot_Z8whJpfK2r{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_Z8whJpfK2r{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_Z8whJpfK2r{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The significance of these organoids extends beyond biological fidelity; they represent a scalable and reproducible solution that mitigates labor-intensive manual methodologies predominant in current research workflows. The precise spatial control afforded by 3D bioprinting enables consistent production of tumor models, significantly expediting the process of preclinical drug screening. Researchers can now rapidly assess the efficacy of multiple therapeutic candidates in parallel, tailoring treatment strategies to the unique genetic and phenotypic profile of an individual’s tumor. This personalized approach promises to transform how nephrologists and oncologists devise treatment regimens, potentially improving clinical outcomes and reducing adverse effects associated with ineffective therapies.
Renal cell carcinoma remains a formidable clinical challenge due to its rising incidence and notorious heterogeneity. Its pathogenesis involves a multitude of genetic aberrations that evolve over time, fostering resistance to chemotherapy and targeted agents, heightening the risk of recurrence and metastasis. Conventional laboratory models struggle to capture this evolving complexity, constraining efforts to develop precision medicine protocols. By contrast, the patient-derived organoids created through this bioprinting platform faithfully preserve mutational landscapes and phenotypic traits, enabling longitudinal studies of tumor evolution and drug resistance mechanisms.
At the heart of this innovation is the meticulous integration of multidisciplinary expertise encompassing mechanical engineering, chemical system engineering, and molecular oncology. Dr. Yuan Pang, Associate Professor at Tsinghua University and co-author of this study, highlights that the ability to mass-produce heterogeneous tumor models “could greatly accelerate the discovery of effective, patient-specific treatments.” The combination of engineering precision and biological authenticity in these organoids provides an essential bridge between bench research and bedside application, epitomizing the ideals of translational medicine.
The implications of this research resonate well beyond RCC, offering a versatile framework applicable to other malignancies characterized by cellular heterogeneity and microenvironmental complexity. The capacity to bioprint organoids maintaining phenotypic fidelity opens new avenues for studying tumor-stroma interactions, immunotherapy responses, and the role of the extracellular matrix in cancer progression. Furthermore, the reduced reliance on animal testing aligns with ethical imperatives, marking progress toward more humane and efficient research methodologies.
This breakthrough also promises to influence pharmaceutical development pipelines. By enabling high-throughput screening of drug candidates on patient-specific tumor constructs, pharmaceutical companies can refine lead compounds earlier in the development process, reducing costs and attrition rates traditionally associated with oncology therapeutics. Additionally, clinicians could leverage such organoids to predict resistance patterns and adapt treatment plans dynamically, a feat previously unattainable with static biopsy samples or generic cell lines.
Moreover, the vascular-like structures incorporated into these bioprinted tumors provide a unique vantage point for studying angiogenesis—the formation of new blood vessels—a hallmark of cancer progression. Understanding how these neovessels interact with cancer cells and facilitate metastasis could inform the development of novel anti-angiogenic therapies that disrupt tumor sustenance and dissemination. This integrated modeling approach thus serves as a powerful investigative tool across multiple dimensions of tumor biology.
Despite these promising advancements, challenges remain. Scaling bioprinting techniques for routine clinical application requires further refinement to ensure reproducibility, cost-effectiveness, and regulatory compliance. Additionally, comprehensive molecular characterization of the printed organoids across diverse RCC subtypes will be essential to validate their utility broadly. Nonetheless, the current progress heralds a new era in personalized oncology research, emphasizing precision, fidelity, and translational relevance.
The study exemplifies the synergy achievable when engineering innovation meets medical necessity, charting a transformative course for kidney cancer research and therapy. As these patient-derived, bioprinted organoids become more integrated into clinical and pharmaceutical workflows, they hold the promise of enabling truly personalized medicine—where treatments are not just designed based on population averages but intricately woven around the unique biological signature of each patient’s tumor.
Subject of Research: Cells
Article Title: Bioprinting of Patient-Derived Heterogeneous Renal Cell Carcinoma Organoids for Personalized Therapy
News Publication Date: 12-Aug-2025
Web References:
https://iopscience.iop.org/article/10.1088/1758-5090/adecc5
References:
Pang, Y., Shou, J., et al. (2025). Bioprinting of Patient-Derived Heterogeneous Renal Cell Carcinoma Organoids for Personalized Therapy. Biofabrication. DOI: 10.1088/1758-5090/adecc5
Image Credits: J-VAR / IOP Publishing
Keywords: Diseases and disorders, Renal Cell Carcinoma, 3D Bioprinting, Personalized Medicine, Tumor Organoids, Cancer Research
Tags: 3D bioprinting technologyadaptive resistance mechanisms in tumorscancer biology advancementsdynamic cellular microenvironmentintratumoral diversity in cancerkidney tumor organoidslimitations of traditional cancer modelspatient-derived tumor modelspersonalized cancer treatment approachesrenal cell carcinoma researchtargeted cancer therapiestherapeutic testing accuracy