Research finds mechanism by which bacterial toxis evolve ability to cause new illnesses
Credit: Mikko Taipale, Roman Melnyk, Jean-Philippe Julien
The coronavirus pandemic is a daily reminder of the consequences brought by a successful invasion of human cells by a pathogen. As new research on bacterial toxins shows, it does not take much for these encounters to turn deadly.
The research has found that two almost identical bacterial toxins cause distinct illnesses–diarrhea and fatal toxic shock syndrome–by binding unrelated human receptors. It also highlights a mechanism by which pathogens have evolved distinct receptor preferences to infect different organs.
“I always think of bacterial toxins as fascinating machines of death in how they find new ways to enter host tissue,” says Mikko Taipale, a co-leader of the study and an assistant professor of molecular genetics in the Donnelly Centre for Cellular and Biomolecular Research at the University of Toronto.
The work was also co-led by Roman Melnyk and Jean-Philippe Julien, both senior scientists at the Hospital for Sick Children in Toronto and associate professors of biochemistry at U of T.
The findings are published in the journal Cell.
Many are familiar with Clostridium difficile, a gut-dwelling bacterium that can cause diarrhea. Lesser known is its close relative, Paeniclostridium sordellii, which too lives in the gut and in female reproductive tract. Infections are rare but fatal and can occur when the bacterial toxin escapes into the bloodstream, during birth for example, and spreads into the lungs and other organs.
Both species are thought to be part of the microbiome, the body’s resident bacteria, but it’s not clear why they harm some people and not others.
The toxin released by C. difficile acts through Frizzled, a cell surface receptor with a role in tissue regeneration. Although P. sordellii produces a similar toxin, it does not bind Frizzled. The nature of its receptor remained unknown and the U of T team decided to find it.
The researchers took an unbiased approach by systematically switching off every gene in human cells and exposing them to the P. sordellii toxin. Cells that survived turned out to lack genes encoding cell surface proteins called semaphorins, and other experiments confirmed that two members of this class, Semaphorin6A and Semaphorin6B, are indeed the receptors for the toxin. Both receptors are present in the lungs as expected, although their role there remains unclear.
Knowing the receptor opens the door to finding treatment. The researchers were able to halt infection in mice by co-injecting the toxin with purified semaphorin fragments, which bound and neutralized the toxin before it could reach the real receptors.
But the finding was unexpected and led to more surprises.
Like Frizzled, semaphorins play important roles in the body, most notably in the developing nervous system where they help guide projecting nerve fibers. That a bacterial toxin impairs lungs through a protein receptor usually found on nerve endings was surprising enough.
But even more surprising was that it binds a receptor with no structural resemblance to Frizzled.
“Here we have two toxins that are so similar to each other, but they use completely different receptors,” says Taipale. “We did not expect to find that.”
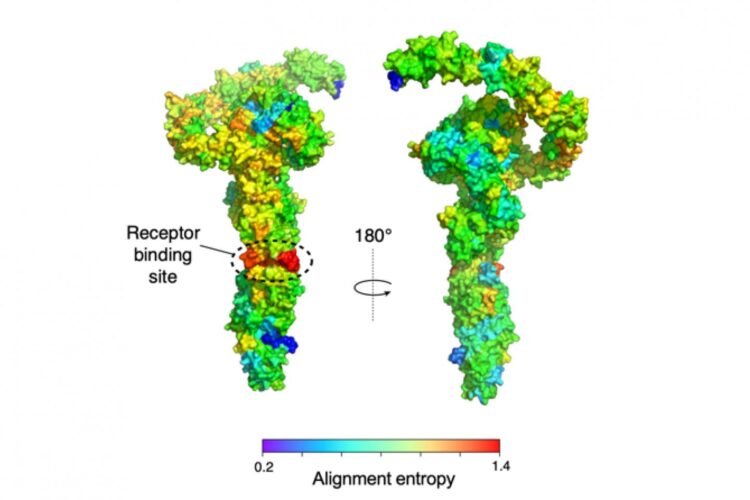
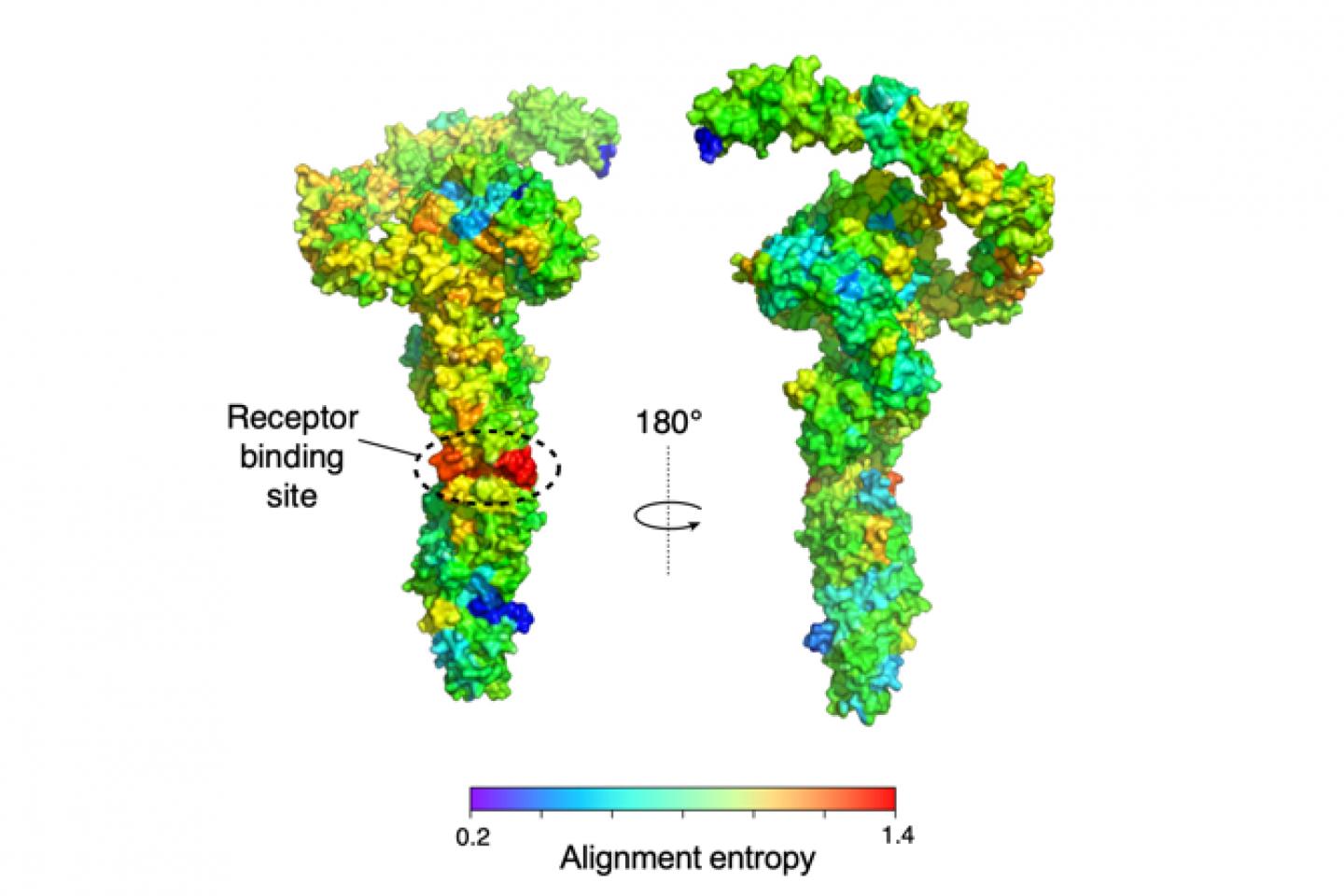
The reason for this is a tiny part of the toxins that differs considerably between C. difficile and P. sordellii. Found in the middle of the toxin, it forms a surface by which both toxins contact their receptors, as revealed by cryo electron microscopy, which allows a detailed three-dimensional view of molecular structure.
Each toxin protein is composed of about 2500 amino-acids and the researchers were able to pinpoint those that directly engage with the receptor. Swapping mere 15 of these amino acids between the two toxins was sufficient to switch receptor preference. In other words, they created a P. sordellii toxin that targeted Frizzled and vice versa.
“We were floored when we saw that the toxins shared a surface each evolved to uniquely interact with distinct cells,” says Julien, who along with Taipale plays for The Flying Puckheads, the hockey team of U of T’s Faculty of Medicine.
It appears that while the rest of the toxin is under strong evolutionary pressure to remain unchanged, the receptor-binding surface is free from such constraints. This can allow toxins to evolve into variants that can bind new receptors to invade other tissues and hosts.
Receptor switching is not unique to bacteria, however. SARS-CoV-2 and coronavirus strains that cause common cold use the same part of the now famous spike protein to bind diverse receptors, which might explain differences in disease severity.
“This is a nice example of how viruses and bacteria – from completely different domains of life — have found similar molecular tactics to change their receptor targets in human cells,” says Taipale. “And it also reminds us how much cool biology one can find in the microbial world!”
###
Media Contact
Jovana Drinjakovic
[email protected]