Early genetic testing can improve cancer outcomes, but individuals often don’t undergo this screening if they lack a family history or can’t afford a test. A clinical laboratory team at Oregon Health & Science University is hoping to change that for residents of their state by providing free genetic screening for inherited cancer and familial hypercholesteremia to all adults with an Oregon address. After screening over 13,000 Oregonians since 2018, the team presents their methods, findings, and lessons learned on July 27 in The American Journal of Human Genetics.
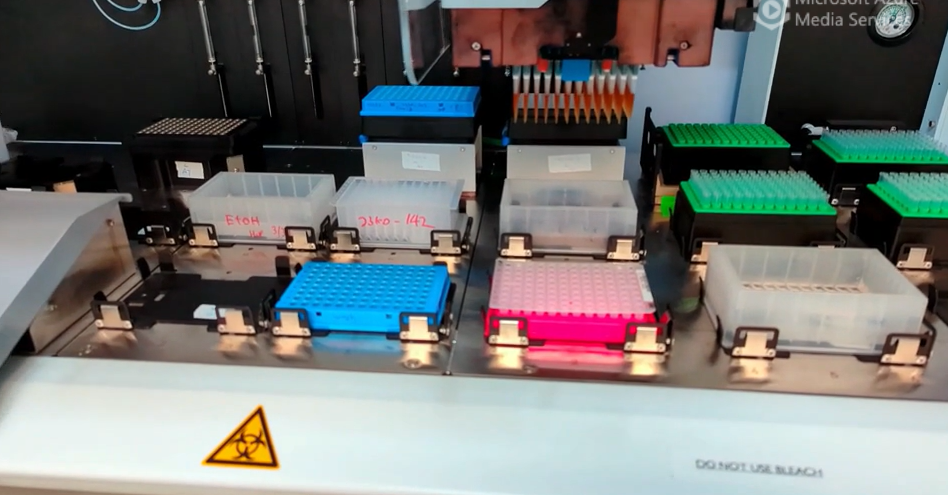
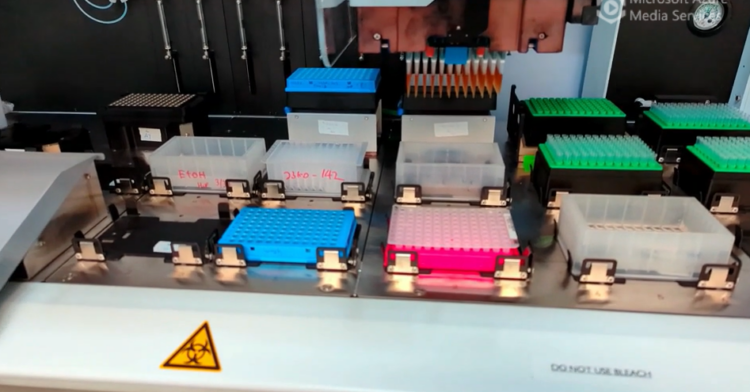
Credit: Gregory Goh
Early genetic testing can improve cancer outcomes, but individuals often don’t undergo this screening if they lack a family history or can’t afford a test. A clinical laboratory team at Oregon Health & Science University is hoping to change that for residents of their state by providing free genetic screening for inherited cancer and familial hypercholesteremia to all adults with an Oregon address. After screening over 13,000 Oregonians since 2018, the team presents their methods, findings, and lessons learned on July 27 in The American Journal of Human Genetics.
“We’re hoping that this can really be used as a model for other states that want to do low-cost population screening,” says first author Timothy O’Brien, a staff scientist at Knight Diagnostic Laboratories. “We’ve provided a kind of roadmap where up-and-coming screening programs can look at us and see both what worked and what could be improved upon.”
The team recruited participants through social media ads and tabling at events like farmers markets. They even set up vending machines where individuals could retrieve and return testing kits that collected a mouthwash saliva sample. After the onset of the COVID-19 pandemic, individuals could request a testing kit through the mail. Once participants gave their consent through a HIPAA-compliant app, samples were processed at a clinical laboratory to screen for disease-causing variants in 31 genes related to inherited cancer and 1 gene related to familial hypercholesteremia.
“We wanted to report on any disease-causing variant that was deemed to be actionable, which means there’s something you can do about it,” says senior author Sue Richards, a Professor Emeritus of Molecular & Medical Genetics at Oregon Health & Science University. “It could be something like changing your screening habits, taking a prophylactic surgery or medication, or consulting with your clinician.”
710 out of over 13,000 participants screened positive for a disease-causing variant. All participants with confirmed positive results received a call from a genetic counselor to explain their results, how the results impact their disease risk, and recommendations for medical management. “Genetic counseling is critical to this program,” says Richards. “It’s not easy for the public to understand these genetic testing reports because they’re fairly technical, and it’s important to understand that just because they carry a disease-causing variant may not mean that they will develop that type of cancer. The counselor also talks to them not only about their own health and family history but also how they pass that information along to other family members, since they are at risk of having the variant as well.”
When the laboratory team first started this project, they had to scale up the lab’s genetic testing workflow to about ten times its original capacity by focusing on a select group of disease-causing variants and employing the help of robots, which performed more tedious tasks. This allowed the group to process up to 1,000 samples per month with one lab technologist at the estimated cost of $50 per participant. To reduce the possibility of a laboratory mix-up resulting in a false positive, all participants with positive results were asked to undergo secondary screening using a different genetic sequencing method. Even so, the researchers report zero clinically relevant sample mix-ups out of the 20,000 specimens that they sequenced.
From their sequencing results, the researchers have also assembled a large repository of data that can be used to analyze the genetic risk factors of Oregon’s population and conduct additional research studies. Approximately 5% of participants screened positive for a disease-causing inherited cancer variant, which was higher than several prior population-screening studies have reported and may be because people with a personal or family history of cancer were more likely to seek testing.
This higher-than-expected prevalence could also be because prior studies screened for a different set of genes. The American College of Medical Genetics and Genomics (ACMG) details a minimum set of genes not related to the individual’s condition but recommended to analyze in those undergoing clinical testing. However, if the researchers had only examined genes from this list, they would have missed 59% of disease-causing variants in their study population. In addition, the most common disease-causing variants detected in the study were not on ACMG’s list. This highlights how expanding the range of genes being tested can have a significant impact on how many people receive positive results in large screening studies.
The team plans on continuing their screening program in the future and increasing efforts to reach a more diverse population of participants. Currently, 76% of study participants are female, so the study is looking at how to recruit more male participants. In addition, by translating their consent app into Spanish, the researchers plan on reaching more of Oregon’s Spanish-speaking population.
“The overall goal of this project was really to help Oregonians and empower them with this health information,” says O’Brien. “We feel like we’ve been able to accomplish that and hope that this continues to be a strong proponent of health for Oregonians in the future.”
###
This work was supported by the Cancer Early Detection Advanced Research Center, Knight Cancer Institute, and National Institutes of Health. Information about conflicts of interest can be found in the text of the paper.
The American Journal of Human Genetics, O’Brien et al. “Population screening shows risk of inherited cancer and familial hypercholesteremia in Oregon” https://www.cell.com/ajhg/fulltext/S0002-9297(23)00239-2
The American Journal of Human Genetics (@AJHGNews), published by Cell Press for the American Society of Human Genetics, is a monthly journal that provides a record of research and review relating to heredity in humans and to the application of genetic principles in medicine and public policy, as well as in related areas of molecular and cell biology. Visit: http://www.cell.com/ajhg. To receive Cell Press media alerts, contact [email protected].
Journal
American Journal of Human Genetics
DOI
10.1016/j.ajhg.2023.06.014
Method of Research
Observational study
Subject of Research
People
Article Title
Population screening shows risk of inherited cancer and familial hypercholesterolemia in Oregon
Article Publication Date
27-Jul-2023