In a groundbreaking investigation into the intersection of regulatory approvals and health insurance coverage, recent research published in JAMA sheds new light on how commercial health plans in the United States navigate coverage decisions for FDA-approved cell and gene therapies. This study reveals a pervasive trend: commercial insurers often impose coverage requirements that exceed the original FDA-approved product labeling. These findings highlight a complex dynamic where insurance policies are not solely reliant on regulatory endorsements but are intricately tied to the strength and scope of clinical evidence underpinning the therapies.
Cell and gene therapies represent one of the most promising frontiers in contemporary medicine, offering the potential for curative treatments for previously intractable diseases. The FDA’s approval process for these therapies is highly rigorous, entailing comprehensive clinical trials designed to establish safety and efficacy. Yet, the real-world dissemination and accessibility of these innovative treatments are heavily influenced by insurance coverage policies. This study elucidates that coverage criteria often reflect a more stringent adherence to pivotal trial parameters rather than the broader FDA label indications, effectively narrowing patient access to those precisely matching trial populations.
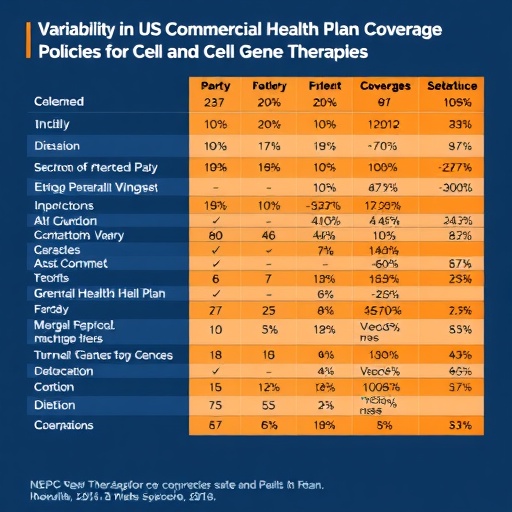
At the core of this research lies a detailed comparative analysis between FDA-approved labels and the coverage policies of commercial health plans. The researchers performed a systematic review of coverage documents for multiple FDA-approved cell and gene therapies, meticulously comparing the stipulated clinical criteria against pivotal trial inclusion and exclusion criteria. This approach allowed for the quantification of discrepancies between regulatory approval and insurance coverage, revealing that many plans require additional documentation or stringent clinical indications before granting coverage.
The implications of these findings are multifaceted. On the one hand, insurers seem to prioritize robust clinical evidence, basing their criteria predominantly on the populations enrolled in pivotal trials, thus potentially safeguarding against off-label use that might lack sufficient empirical support. On the other hand, this conservative stance could inadvertently restrict broader patient access to these transformative treatments, especially for populations who might benefit but fall outside narrowly defined trial criteria.
The methodology employed in this study integrates aspects of health policy analysis with clinical medicine, distinguishing itself by blending empirical data from insurance coverage policies with detailed FDA documentation. The researchers emphasize that while regulatory approval constitutes a significant milestone, it does not guarantee uniform insurance coverage. Instead, insurers exercise independent judgment that reflects an implicit risk-benefit calculus grounded in evidence strength.
Notably, the study underscores the dynamic relationship between regulatory science and payer decision-making. While the FDA mandates stringent clinical trials to assess drug safety and efficacy before approval, insurers operate within financial and clinical risk management frameworks that may call for even tighter controls. Such policies may require additional patient diagnostics, confirmation of disease severity, or prior authorization steps aligned with trial-specific criteria, ensuring that coverage aligns closely with demonstrated therapeutic benefit.
Furthermore, this trend reflects broader systemic challenges in integrating cutting-edge therapies into existing healthcare infrastructure. The high costs associated with cell and gene therapies necessitate judicious coverage policies to balance innovation with system sustainability. Insurance payers appear to rely heavily on clinical trial evidence, using it as a benchmark to mitigate financial and clinical uncertainties surrounding widespread adoption.
This meticulous study also brings to the forefront discussions about real-world evidence (RWE) and its role in supplementing clinical trial data. While FDA approvals may evolve to incorporate RWE as a component of ongoing evaluation, payer policies currently remain anchored to initial pivotal trial criteria. The lag in adaptation underscores an area ripe for policy harmonization to enhance patient access without compromising evidentiary standards.
Moreover, the research draws attention to potential equity considerations. Populations underrepresented in clinical trials—such as minorities, elderly patients, or those with comorbidities—might face disproportionate barriers under these insurance coverage frameworks. By tethering coverage decisions tightly to pivotal trial criteria, payers may inadvertently exacerbate disparities in access to novel treatments, an issue warranting urgent attention from policymakers and stakeholders.
The study further invites discourse on the necessity for greater transparency and standardization in coverage decision-making processes. Given the heterogeneity observed across commercial insurers, patients and providers often confront confusion and unpredictability regarding coverage eligibility. Enhancing clarity and aligning coverage with evolving scientific evidence could foster improved healthcare delivery and patient outcomes in the rapidly evolving field of cell and gene therapy.
An additional dimension touched upon in this investigation is the role of cost-effectiveness assessments. Although not the primary focus, the interplay between clinical evidence and economic evaluation shapes insurance coverage strategies. Payors appear to be balancing the promise of long-term clinical benefit against immediate financial outlays, often prioritizing patients who meet strict trial parameters where efficacy is most strongly demonstrated.
Importantly, the corresponding author, Dr. James D. Chambers of Tufts Medical Center, emphasizes that these findings represent an essential step towards understanding how evidence translates—or fails to translate—into coverage policies. The study serves as a foundation for future research aimed at optimizing payer frameworks to foster more equitable and evidence-based access to next-generation therapies.
In conclusion, this pioneering research articulates a nuanced portrait of the insurance coverage landscape for FDA-approved cell and gene therapies, revealing that commercial health plans generally adopt eligibility criteria reflective of pivotal trial design rather than broad regulatory labeling. This alignment with stronger supporting evidence underscores both opportunities and challenges in ensuring access to life-changing therapies amidst complex financial, clinical, and policy considerations. As the field advances, ongoing dialogue between regulators, payers, clinicians, and patients will be crucial to harmonize evidence-based innovation with accessible care.
Subject of Research: Insurance coverage policies for FDA-approved cell and gene therapies and their alignment with pivotal trial criteria.
Article Title: (Information not provided)
News Publication Date: (Information not provided)
Web References: (No URLs provided)
References: doi:10.1001/jama.2025.15148
Image Credits: (Information not provided)
Keywords: Gene therapy, United States population, Health insurance