SAN ANTONIO, Feb. 4, 2026 – Stroke survivors frequently confront a debilitating aftermath that extends beyond the initial cerebrovascular insult—post-stroke spasticity. This complex neurological condition, characterized by persistent muscle hypertonia and involuntary spasms, often goes underrecognized and undertreated in the critical early stages of recovery. Emerging research now indicates that the traditional view of spasticity as an inevitable consequence of stroke significantly underestimates the potential for intervention. Scientists and clinicians alike are calling for a paradigm shift toward early detection and targeted therapies to mitigate the profound impact of spasticity on functional recovery.
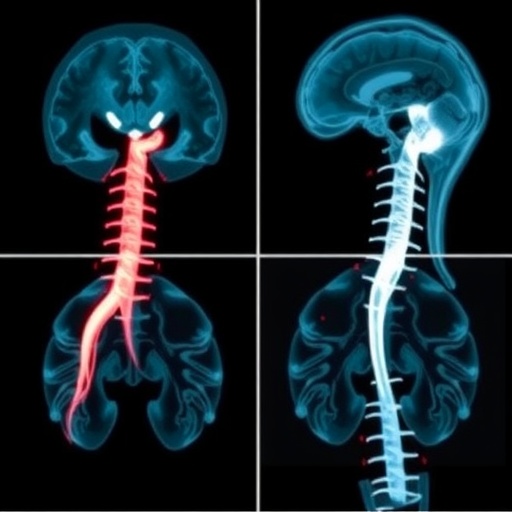
Post-stroke spasticity manifests as abnormal muscle stiffness due to lesions within central motor pathways, principally arising from ischemic or hemorrhagic injury to the brain. The resulting increase in muscle tone disrupts normal neuromuscular control, impairing voluntary movement and severely limiting patients’ ability to perform activities of daily living. Importantly, spasticity contributes not only to motor impairment but also to secondary complications such as chronic pain, joint contractures, and compromised skin integrity. Epidemiological estimates indicate that between 30% and 80% of stroke survivors develop spasticity to varying degrees, highlighting a significant clinical burden that extends beyond acute stroke management.
Recent advancements in neurorehabilitation underscore the critical importance of early identification of spasticity, often within the initial three months following stroke onset. This early window represents a period of heightened neuroplasticity, during which the central nervous system retains an enhanced capacity for functional reorganization and recovery. Multimodal approaches integrating precise biomechanical assessment, neuroimaging techniques, and electrophysiological monitoring offer promising avenues for early diagnosis. Timely intervention during this phase can prevent maladaptive muscle changes and preserve biomechanical function, thereby improving long-term motor outcomes.
The American Heart Association’s newly published scientific statement, spearheaded by leading neurologists from UT Health San Antonio, delineates a comprehensive framework for proactive spasticity management. This document synthesizes evidence from cutting-edge neuroscience, rehabilitation science, and clinical trials to advocate for coordinated, multidisciplinary care pathways. Such pathways emphasize the integration of pharmacological agents—like botulinum toxin and oral antispastic drugs—with physical modalities, including task-specific training, neuromuscular electrical stimulation, and advanced robotic-assisted therapies. By harmonizing these strategies, clinicians can tailor interventions to the individual’s evolving clinical profile.
Moreover, the statement highlights the profound disparities in access to specialized post-stroke rehabilitation, particularly in under-resourced rural settings. These inequities contribute to delayed diagnosis and suboptimal management of spasticity, compounding disability and reducing quality of life. Telemedicine platforms and innovative care delivery models emerge as pivotal solutions to bridge these gaps. By leveraging remote monitoring and virtual rehabilitative exercises guided by specialists, patients in geographically isolated regions can receive timely and effective spasticity care, fostering equitable outcomes across diverse populations.
From a pathophysiological perspective, spasticity involves alterations in descending inhibitory pathways and increased excitability of the stretch reflex arc at the spinal level. Molecular mechanisms implicate changes in synaptic transmission, neuromodulator imbalances, and neuroinflammatory processes following ischemic injury. These insights provide a rationale for targeted pharmacological interventions aimed at modulating neurotransmitter systems and inflammatory cascades, suggesting a potential role for novel agents in future therapeutic algorithms.
Functional neuroimaging studies, including diffusion tensor imaging, have elucidated the structural integrity of corticospinal tracts and their correlation with spasticity severity. Such objective biomarkers facilitate the stratification of patients based on risk profiles, enabling personalized rehabilitation protocols. The integration of wearable sensor technologies further enhances the capacity for continuous monitoring of spasticity-induced motor dysfunction in naturalistic environments, offering real-time data to adjust therapeutic plans dynamically.
Interdisciplinary collaboration among neurologists, physiatrists, physical therapists, and occupational therapists forms the cornerstone of optimal post-stroke spasticity management. Shared decision-making involving patients and caregivers is critical to align rehabilitative goals with patient-centered outcomes. Educational initiatives aimed at increasing awareness of spasticity’s implications and available interventions are essential components in transforming current clinical practice.
Furthermore, advances in regenerative medicine and neuromodulation hold promise for future spasticity treatment paradigms. Techniques such as stem cell therapy, transcranial magnetic stimulation, and deep brain stimulation are under investigation for their capacity to modulate neural circuits and promote motor recovery. Early clinical trials demonstrate potential benefits, suggesting that these innovative therapies could complement established approaches within comprehensive care models.
The collective evidence underscores that spasticity is not merely a static consequence of stroke but a dynamic, modifiable condition amenable to early and targeted intervention. Embracing this perspective fosters optimism toward improving functional independence and quality of life among millions of stroke survivors worldwide. The American Heart Association’s scientific statement serves as a clarion call to the medical community, urging heightened vigilance and proactive strategies in the fight against post-stroke spasticity.
UT Health San Antonio continues to lead groundbreaking research initiatives focused on neural repair and rehabilitation, driven by a commitment to advancing clinical science and translating discoveries into improved patient care. The upcoming International Stroke Conference 2026 will feature presentations that delve deeper into therapeutic innovations and case studies, facilitating dissemination of best practices and fostering global collaboration in stroke recovery.
This transformative approach to post-stroke spasticity represents a convergence of technological innovation, interdisciplinary expertise, and patient-centered care philosophy. By realizing the full potential of early diagnosis and multimodal treatment, healthcare systems can achieve substantial reductions in long-term disability and associated socioeconomic burdens. Ultimately, these efforts embody the aspiration that stroke recovery can be not only prolonged survival but also meaningful restoration of function and dignity.
Subject of Research: Post-stroke spasticity and its early recognition and intervention
Article Title: Early Recognition and Intervention for Poststroke Spasticity: A Scientific Statement from the American Heart Association
News Publication Date: January 29, 2026
Web References:
Early Recognition and Intervention for Poststroke Spasticity – Stroke Journal DOI
Top Things to Know: Early Recognition & Intervention for Poststroke Spasticity
References:
Bandela S, McPherson L, Harvey RL, Awosika O, Aggarwal D, Liu CY, Raghavan P, Goldberg MP. Early Recognition and Intervention for Poststroke Spasticity: A Scientific Statement from the American Heart Association. Stroke. 2026 Jan 29; doi:10.1161/STR.0000000000000515.
Keywords: Brain ischemia, Muscle contraction, Pain, Heart, Heart disease, Cardiovascular disease
Tags: American Heart Association guidelines on spasticitychallenges in diagnosing post-stroke spasticityclinical management of post-stroke spasticityearly detection of post-stroke spasticityimpact of spasticity on stroke recoveryimportance of targeted therapies for spasticityinterventions for post-stroke complicationsmuscle hypertonia in stroke patientsneurological conditions after strokerole of neurorehabilitation in stroke recoverystroke rehabilitation strategiestreatment options for post-stroke spasticity