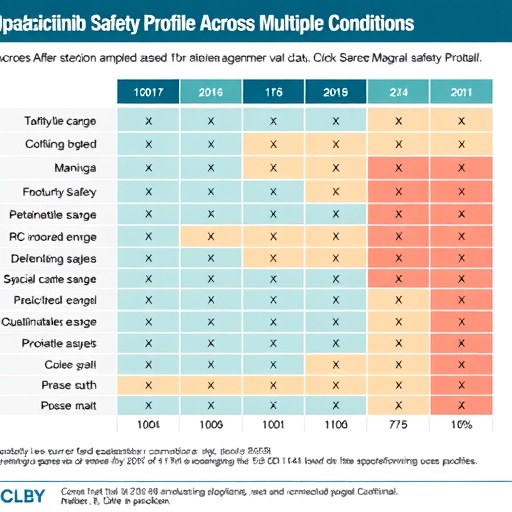
In recent years, the emergence of Janus kinase (JAK) inhibitors has revolutionized the treatment landscape for various autoimmune disorders, including rheumatoid arthritis, psoriatic arthritis, and inflammatory bowel disease. Among these therapeutic agents, Upadacitinib has garnered significant attention due to its compelling efficacy and safety profile. A comprehensive descriptive analysis published in Adv Ther has provided critical insights into the safety of Upadacitinib across a diverse range of conditions. This analysis aggregates data spanning over 27,000 patient-years, presenting an invaluable resource for both clinicians and patients.
The meticulous study was conducted by a multidisciplinary team led by esteemed researchers including Burmester, Deodhar, and Irvine. They systematically reviewed the safety outcomes from multiple clinical trials, harnessing vast data pools to assess adverse events, their frequencies, and the overall tolerability of Upadacitinib across different patient populations. This large-scale analysis stands as a cornerstone of evidence for the safety of JAK inhibitors, particularly as they become more widely prescribed in clinical practice.
One of the key findings from the analysis indicates that Upadacitinib exhibits a safety profile that is generally consistent with expectations based on previously published data. Among the various adverse events assessed, the most notable were infections, which occurred at a rate that reflects the inherent risk associated with immunosuppressive therapies. However, it is crucial to contextualize these findings within the framework of the diseases being treated, as the baseline risk of infections often differs between patient groups.
The study also delves into the specifics of serious adverse events (SAEs), shedding light on their incidence rates in a population that spans several autoimmune diseases. Interestingly, while Upadacitinib was associated with some SAEs, the overall rates remained relatively low when considering the extensive duration of exposure across thousands of patient-years. This reassurance provides a critical argument for the continued use of Upadacitinib, particularly for patients with complex and refractory conditions who require robust treatment options.
On the subject of cardiovascular safety, the analysis further confirms that Upadacitinib does not appear to significantly increase the risk of cardiovascular events compared to traditional therapies. Given the heightened cardiovascular risks associated with chronic inflammatory states, this finding is particularly relevant, potentially offering a more favorable profile for patients with underlying cardiac conditions who might otherwise be sidelined from aggressive therapy.
In terms of laboratory abnormalities, the researchers meticulously cataloged changes in hematological parameters, liver enzymes, and lipid levels. Their findings indicated that while some laboratory abnormalities were noted, most were transient and not associated with clinically significant complications. This understanding is vital for practicing physicians when weighing the benefits of Upadacitinib treatment against potential risks, especially in long-term management scenarios where monitoring of lab values is critical.
Throughout the comprehensive evaluation, the researchers also emphasized the importance of individualized treatment approaches. They advocate for a nuanced understanding of each patient’s unique risk factors and comorbidities, suggesting that shared decision-making is paramount. As physicians engage in discussions with patients regarding the initiation of Upadacitinib therapy, a well-rounded comprehension of both the potential benefits and risks is essential for optimizing treatment outcomes.
In addition to examining the safety of Upadacitinib, the analysis reviews emerging data concerning its efficacy. Clinical outcomes indicate that Upadacitinib is not only effective in achieving symptom relief but also in improving the quality of life for patients suffering from debilitating autoimmune conditions. This dual advantage positions Upadacitinib as a formidable option in the therapeutic arsenal against chronic inflammatory diseases.
The findings from this analysis will undoubtedly spark further investigations into the long-term safety and efficacy of Upadacitinib. As patient populations expand and follow-up periods lengthen, ongoing research will be crucial in determining the role of JAK inhibitors in the evolving landscape of autoimmune disease management. Moreover, the juxtaposition of Upadacitinib with other therapeutic modalities will allow for a richer understanding of how best to tailor treatments for diverse patient profiles.
Ultimately, the publication serves as a testament to the ongoing evolution in the field of rheumatology and beyond. With each new study, we inch closer to delivering safer and more effective treatments for the millions affected by autoimmune diseases. The high-level synthesis of safety data presented in this analysis equips physicians with the knowledge required to make informed decisions in the best interest of their patients.
The future of autoimmune disease treatment will undoubtedly include a more significant role for agents like Upadacitinib, especially as new formulations and dosing regimens are explored. For patients, this means an increasingly diverse array of options, each with unique benefits and safety considerations. Thus, the need for continued vigilance and research is paramount as we aim to refine therapies that enhance healing while minimizing risk.
As we look towards the horizon in autoimmune research, the insights gleaned from this pivotal analysis will not only guide current practice but will also inspire future inquiries into innovative therapeutic strategies, ensuring that patients have access to the best possible care. Through the collaborative efforts of researchers, clinicians, and patients alike, the landscape of autoimmune disease management continues to transform, offering renewed hope for many who suffer from these chronic conditions.
In conclusion, the comprehensive safety profile of Upadacitinib highlighted in this analysis marks a pivotal moment in the management of autoimmune diseases. As we continue to explore the complexities of therapeutic interventions in these conditions, the data serve as a foundation for informed decision-making that prioritizes patient health outcomes while leveraging the potential benefits of novel treatments.
Subject of Research: Safety Profile of Upadacitinib in Autoimmune Diseases
Article Title: Safety Profile of Upadacitinib: Descriptive Analysis in Over 27,000 Patient-Years Across Rheumatoid Arthritis, Psoriatic Arthritis, Axial Spondyloarthritis, Atopic Dermatitis, and Inflammatory Bowel Disease
Article References: Burmester, G.R., Deodhar, A., Irvine, A.D. Safety Profile of Upadacitinib: Descriptive Analysis in Over 27,000 Patient-Years Across Rheumatoid Arthritis, Psoriatic Arthritis, Axial Spondyloarthritis, Atopic Dermatitis, and Inflammatory Bowel Disease. Adv Ther (2025). https://doi.org/10.1007/s12325-025-03328-y
Image Credits: AI Generated
DOI: 10.1007/s12325-025-03328-y
Keywords: autoimmune diseases, Upadacitinib, safety profile, JAK inhibitors, clinical trials
Tags: adverse events frequency analysisautoimmune disorder treatment landscapeclinical trial safety outcomesevidence-based medicine for JAK inhibitorsinflammatory bowel disease therapiesJAK inhibitors in autoimmune disorderslarge-scale safety data analysismultidisciplinary research on Upadacitinibpatient population tolerabilitypsoriatic arthritis managementrheumatoid arthritis treatmentUpadacitinib safety profile



