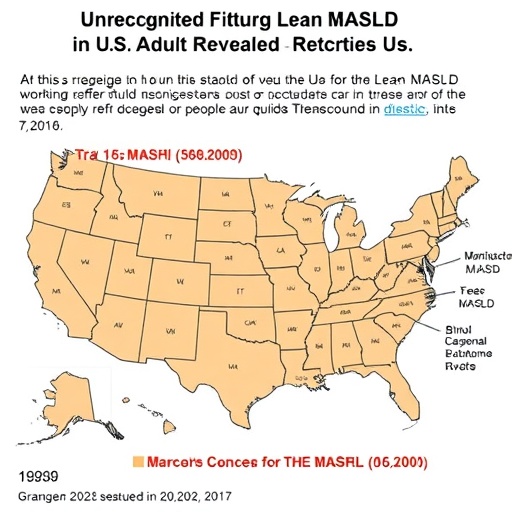
Recent research has unveiled a concerning aspect of health in the United States, particularly focusing on lean metabolic dysfunction-associated steatotic liver disease (MASLD). This study, spearheaded by a team of researchers including Njei et al., highlights the unrecognized prevalence of lean MASLD among U.S. adults, which appears to be largely underestimated and undiagnosed. The findings emerged from data acquired through the National Health and Nutrition Examination Survey (NHANES) during the years 2017 to 2020, providing a crucial insight into this growing health concern.
The significance of this research lies not only in the startling prevalence of lean MASLD but also in its implications for public health. Traditionally, metabolic dysfunction-associated liver diseases have been associated with obesity and overweight individuals. However, this study challenges this perception by identifying a substantial number of individuals with lean MASLD who do not fit the typical demographic. This population, often overlooked in clinical assessments, may suffer from analogous health risks yet remain undiagnosed.
A key facet of the research involved a thorough examination of metabolic features associated with lean MASLD. The researchers meticulously analyzed the metabolic parameters within the participant cohort from NHANES, emphasizing the importance of understanding the implications of body composition in metabolic health. The analysis illuminated the metabolic disturbances common in individuals diagnosed with lean MASLD, showcasing that lean individuals can also experience detrimental liver health associated with metabolic syndrome components such as insulin resistance, dyslipidemia, and systemic inflammation.
There is an urgent need to revise the current approach towards diagnosing and treating liver diseases. The traditional view that associates liver health exclusively with obesity must evolve to accommodate findings such as those presented in this research. The fact that lean individuals can harbor significant liver fat accumulation and metabolic derangements indicates a paradigm shift in our understanding of liver disease risk factors.
Moreover, the genetic and environmental contributions to lean MASLD are intricate and merit further exploration. The interplay between genetic predispositions and lifestyle factors such as diet and physical activity is crucial in understanding why certain lean individuals develop MASLD. Environmental elements including exposure to toxins and the microbiome may also play a role, adding layers of complexity to the research landscape surrounding liver diseases.
Healthcare practitioners must become more vigilant in identifying potential cases of lean MASLD. This initiative involves refining screening practices and educating healthcare providers about the potential of a masked epidemic lurking within seemingly healthy demographics. The implementation of targeted screening protocols could aid in early detection, enabling timely interventions that could mitigate long-term health impacts.
The broader implications of this study transcend individual health outcomes. The undiagnosed burden of lean MASLD poses significant challenges to healthcare systems, particularly as healthcare costs continue to escalate. Addressing the diagnostic gaps in liver health is paramount not just for individual recovery but also for the sustainability of healthcare resources.
In terms of treatment avenues, emerging perspectives suggest that lifestyle modifications can play a critical role in managing lean MASLD. This includes nutritional counseling, fostering physical activity, and fostering a supportive environment that encourages healthier choices. Nevertheless, further research is needed to solidify the efficacy of these interventions specifically tailored to populations affected by lean MASLD.
Critically, patient education is a vital component of any intervention strategy. Empowering individuals with knowledge about their health risks, specifically regarding lean MASLD, can motivate them to seek appropriate care and adopt healthier lifestyles. As individuals become more informed and proactive about their health, there is potential for positive change at both personal and community levels.
The intersection of clinical practice, public health policies, and research cannot be overstated in addressing the rising tide of lean MASLD. Collaborative efforts among researchers, healthcare providers, and public health officials are essential to ensure that those at risk receive the necessary support and resources. Identifying lean MASLD earlier could transform treatment approaches and improve health outcomes significantly.
In conclusion, the research by Njei et al. sheds light on a significant yet often overlooked health issue—increasing awareness about lean MASLD in U.S. adults is crucial for public health initiatives. This evolution in understanding metabolic liver diseases emphasizes the importance of inclusive diagnostic practices and tailored treatment plans that consider diverse patient demographics. It is imperative that all stakeholders realize the importance of addressing this hidden burden of disease to foster a healthier future for all U.S. adults.
The findings from this study not only challenge our existing knowledge regarding liver diseases but also reshape the narrative surrounding metabolic health. As the medical community embraces this emerging awareness about lean MASLD, we pave the way for significant advancements in prevention, diagnosis, and treatment focused on a broader population spectrum.
Subject of Research: Lean metabolic dysfunction-associated steatotic liver disease (MASLD) in U.S. adults.
Article Title: Lean MASLD in U.S. Adults: Undiagnosed Burden and Metabolic Features from NHANES 2017–2020.
Article References:
Njei, B., Boateng, S., Mohamed, M. et al. Lean MASLD in U.S. Adults: Undiagnosed Burden and Metabolic Features from NHANES 2017–2020.
J GEN INTERN MED (2025). https://doi.org/10.1007/s11606-025-10086-8
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11606-025-10086-8
Keywords: Lean MASLD, metabolic syndrome, liver disease, public health, NHANES, healthcare, diagnosis, treatment.
Tags: body composition and metabolic healthchallenges in diagnosing lean MASLDhealth risks of lean MASLDlean metabolic dysfunction-associated steatotic liver diseasemetabolic health in non-obese individualsmetabolic parameters in liver healthNational Health and Nutrition Examination Survey findingsprevalence of lean MASLDpublic health implications of lean MASLDresearch on liver disease trends in the U.S.underdiagnosed liver diseasesunrecognized health issues in U.S. adults