In a breakthrough study poised to recalibrate neonatal care, researchers have illuminated the complex interplay of iron homeostasis in twin anemia polycythemia sequence (TAPS), a rare but clinically significant condition affecting monochorionic twins. This intricate disorder, where one twin exhibits profound anemia while the other suffers from polycythemia, has long puzzled neonatologists regarding its precise pathophysiological mechanisms and systemic repercussions. Now, the latest research synthesizes a detailed understanding of iron dynamics in both donor and recipient twins, shedding light on the dual risks of iron deficiency and iron overload respectively.
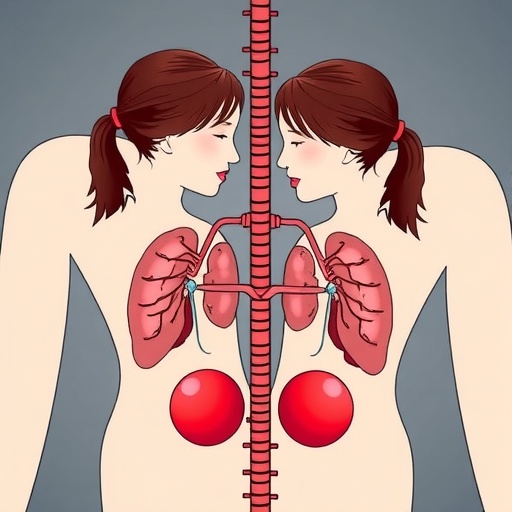
Twin anemia polycythemia sequence occurs due to unbalanced blood flow between monochorionic twins through vascular anastomoses in the shared placenta. This imbalance precipitates one twin becoming severely anemic with low hematocrit levels, while the other develops polycythemia, characterized by abnormally elevated red blood cell counts. The implications of this condition extend beyond circulatory discrepancies and touch on fundamental iron metabolism, a critical determinant of neonatal health. Iron, a vital micronutrient essential for erythropoiesis and neurodevelopment, must be meticulously regulated to avoid detrimental outcomes such as neurotoxicity or developmental delays.
The recent investigation utilized advanced hematological assays and iron panel evaluations to contrast the iron status of donors and recipients in a cohort of TAPS cases. Their findings denote a pronounced risk of iron depletion in anemic donor twins, a direct consequence of their decreased hematologic mass and potential iron loss through selective hemolysis and impaired erythropoiesis. Contrarily, recipient twins manifest increased susceptibility to iron overload, a phenomenon linked to excessive erythrocyte proliferation and iron accumulation, which can catalyze oxidative stress and tissue damage.
.adsslot_5mJwlgVSEq{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_5mJwlgVSEq{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_5mJwlgVSEq{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Crucially, the study underscores that iron dysregulation in TAPS is not merely a secondary symptom but a pivotal factor influencing clinical outcomes and therapeutic decision-making. Traditional interventions, such as intrauterine transfusions, aim to correct hematologic imbalances but may inadvertently exacerbate iron imbalances if not carefully modulated. Thus, continuous monitoring of iron biomarkers becomes indispensable for personalized perinatal management and prevention of iron-related morbidities.
From a mechanistic standpoint, the divergent iron statuses reflect the underlying pathophysiology of TAPS. Donor twins endure a state of hypoxia-induced erythropoietin overproduction, attempting to compensate for anemia but hindered by limited iron availability. Recipient twins, meanwhile, undergo paradoxical polycythemia with increased red cell mass, consequentially sequestering abundant iron. The placental vascular arrangements facilitating unidirectional transfusion likely exacerbate these contrasting iron dynamics, creating a microenvironment of iron disparity.
What makes these revelations particularly compelling is their implication for neurodevelopmental trajectories in affected twins. Iron deficiency in donors can compromise myelination and neurotransmitter synthesis, risking cognitive and motor impairments. In recipients, iron overload potentially catalyzes free radical generation, lipid peroxidation, and neuroinflammation, further underscoring the importance of vigilant iron balance. Therefore, the clinical surveillance protocols must integrate neurodevelopmental follow-up alongside hematologic assessments.
Beyond pathophysiology, the research advocates for novel biomarkers and diagnostic tools tailored to early detection of iron imbalances in TAPS. Incorporating quantitative ferritin measurements, transferrin saturation indices, and erythrocyte indices into routine evaluations could redefine prognostic frameworks. Furthermore, the study opens avenues for exploring adjunctive therapies, such as chelation in recipients or targeted iron supplementation in donors, though such approaches demand rigorous clinical trials to ascertain efficacy and safety.
The interplay between placental biology and fetal iron metabolism revealed in this work invites a reconsideration of prenatal care strategies. It prompts inquiry into the timing and dosage of interventions to optimize iron delivery and prevent sequelae. Personalized medicine approaches, utilizing genetic and epigenetic profiling, may in the future enable tailored iron management protocols, safeguarding the delicate developmental equilibrium in monochorionic twins.
This research also carries implications for postnatal management in neonatal intensive care units. Knowledge of preexisting iron status can guide transfusion practices, nutritional supplementation, and monitoring for iron-induced organ toxicity. The paradigm shift proposed seeks to align perinatal hematology with metabolic stewardship, emphasizing prevention of both deficiency and overload to improve survival rates and quality of life for this vulnerable population.
Moreover, the elucidation of iron homeostasis in TAPS contributes to broader scientific discussions about fetal iron trafficking and regulation under pathological conditions. It deconstructs traditional notions of iron as a passive substrate, highlighting its active role in modulating erythropoiesis and organ development within an interconnected maternal-fetal-medical framework. This insight enriches our comprehension of fetal physiology and pathologies beyond twin gestations.
Ethical considerations emerge in balancing intervention benefits against potential risks. The need for delicate calibration of iron levels demands multidisciplinary collaboration among obstetricians, neonatologists, hematologists, and researchers. Ethical frameworks must guide decision-making to prioritize neonatal wellbeing while respecting parental autonomy and informed consent in complex clinical scenarios.
Ultimately, the study’s findings reverberate beyond the academic sphere, signaling an urgent call to incorporate iron metabolism into clinical algorithms for TAPS. As neonatal survival in complicated monochorionic twin pregnancies improves globally, addressing iron-related complications constitutes a critical frontier in perinatal medicine. These insights foster hope for refined care models that integrate hematologic precision with developmental safeguarding.
The research team’s comprehensive approach, combining clinical data, laboratory analysis, and conceptual synthesis, paves the way for future inquiries into therapeutic innovation. Bridging fundamental science with translational potential, their work exemplifies the evolving interface of perinatal pathology and metabolic regulation. As the community digests these findings, collaborative efforts will be necessary to implement findings into guidelines and practice.
In conclusion, this landmark study reshapes understanding of twin anemia polycythemia sequence by delineating the dual risks of iron deficiency and overload inherent to donors and recipients. It challenges existing paradigms and invites clinicians to adopt nuanced perspectives on iron management in neonatal care. Leveraging emerging biomarkers and therapeutic strategies can mitigate adverse outcomes, safeguard neurodevelopment, and improve prognoses for monochorionic twins facing this complex condition.
As perinatal medicine advances, the integration of iron metabolism into the conceptual framework of TAPS promises to enhance individualized treatment plans. This research exemplifies the critical intersection of hematology, neonatology, and developmental biology, reinforcing the imperative to view iron not merely as a nutrient but as a pivotal determinant of neonatal health in the context of twin gestations.
Subject of Research: Twin anemia polycythemia sequence and its implications on iron metabolism in monochorionic twins.
Article Title: Twin anemia polycythemia sequence and the risk of iron deficiency in donors and iron overload in recipients.
Article References:
Rondagh, M., van de Sande, M.J.A., Tollenaar, L.S.A. et al. Twin anemia polycythemia sequence and the risk of iron deficiency in donors and iron overload in recipients. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02386-y
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41372-025-02386-y
Tags: erythropoiesis in twin pregnancieshematological assays for neonatesiron deficiency risksiron homeostasis in twinsiron metabolism in newbornsiron overload consequencesmonochorionic twin complicationsneonatal care advancementsneurodevelopment and iron balancepathophysiology of TAPStwin anemia polycythemia sequencevascular anastomoses in twins