In the rapidly evolving landscape of diabetes management, recent research reveals critical insights into the usage patterns of SGLT2 inhibitors and GLP-1 receptor agonists among patients suffering from chronic kidney disease (CKD) and type 2 diabetes. A comprehensive study published by Johannes et al. in the journal “Diabetes Therapy” outlines noteworthy temporal changes in the prescription and utilization of these two classes of medications over the span of more than a decade, from 2012 to 2023. Given the increasing prevalence of diabetes and its complications, understanding the shifts in treatment strategies is paramount for optimizing patient outcomes.
The study underscores the pivotal role that SGLT2 inhibitors and GLP-1 receptor agonists have assumed in diabetes management. Initially introduced for their glucose-lowering effects, these medications have demonstrated a broader spectrum of benefits, particularly in patients with concurrent kidney issues. Their unique mechanisms of action not only target hyperglycemia but also provide cardioprotective and nephroprotective effects, which have led to their burgeoning popularity in clinical practice. The research examines the implications of these evolving treatment paradigms within the context of rising diabetes incidences and the growing recognition of the significance of cardiovascular and renal health in this patient demographic.
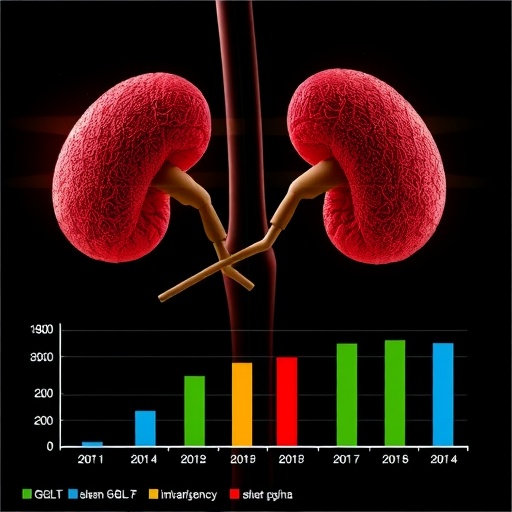
Throughout the study period, the authors observed significant growth in the adoption rates of both SGLT2 inhibitors and GLP-1 receptor agonists among the specified cohort. This trend mirrors the increasing body of evidence supporting the efficacy of these agents in reducing adverse cardiovascular and renal outcomes, an area of acute importance given that diabetes is a major risk factor for kidney disease and cardiovascular events. The researchers collected and analyzed data from a large U.S. patient cohort, offering a granular view of prescribing trends that reflect the shifting landscape of diabetes therapeutics.
One of the most striking conclusions drawn by the researchers is the notable increase in the use of SGLT2 inhibitors, particularly in individuals with more advanced stages of CKD. This trend is reflective of the evolving understanding within the medical community regarding the significance of early intervention with these drugs to mitigate the progression of renal decline. The findings suggest a potential shift toward a more proactive approach in the management of kidneys in diabetic patients, where the use of nephroprotective agents becomes a standard practice rather than an afterthought.
Conversely, the uptake of GLP-1 receptor agonists also saw a considerable rise, although this increase was less dramatic compared to their SGLT2 counterpart. The researchers speculate that the slower adoption may be attributed to several factors, including prescribing habits, patient education regarding the benefits of these medications, and potential barriers such as cost and access to newer therapies. Nevertheless, the overall trend points toward a gradual acceptance of GLP-1 agonists as essential tools in the diabetes management arsenal, particularly for patients seeking weight management alongside glycemic control.
Statistical analysis embedded in the research discourse presents compelling evidence of the changing demographics within the studied population. The data illustrated a noteworthy demographic shift toward a younger patient cohort, which may be indicative of a burgeoning awareness among healthcare providers about the importance of addressing diabetes early in its course. This trend emphasizes the necessity for continuous education and awareness programs targeting both healthcare professionals and patients alike, to ensure that these life-saving medications are utilized optimally.
The implications of these findings extend beyond prescriptive practices; they urge a reflection on healthcare policies that govern the access and affordability of diabetes therapies. Access to these innovative treatments remains uneven, often dictated by insurance formularies and socio-economic challenges that can hinder patient compliance. The research advocates for a concerted effort to devise strategies that streamline access to SGLT2 inhibitors and GLP-1 receptor agonists, delineating the importance of equitable healthcare in alleviating the burden of diabetes complications.
As the research points toward an increasing acceptance of these agents in standard clinical practice, it also raises important questions regarding the long-term sustainability of such trends, particularly as new medications continue to enter the market. Ongoing research will be crucial in understanding how these innovations can be best integrated into therapeutic regimens without compromising patient safety or increasing healthcare costs.
Moreover, patient adherence remains a critical area of concern, as the complexity of diabetes management can often lead to difficulties in maintaining consistent medication regimens. Strategies such as patient-centered education, regular follow-ups, and the integration of digital health solutions may prove invaluable in enhancing medication adherence and ultimately achieving better patient outcomes.
The findings from Johannes et al. serve as a clarion call for the medical community to continue prioritizing research focused on understanding the nuances of diabetes treatment adherence. The evolution of diabetes care hinges on not only prescribing the most effective therapies but also empowering patients through education, awareness, and support to optimize their treatment plans. As researchers and clinicians move forward, fostering a collaborative dialogue amongst all stakeholders will be essential in advancing the care paradigm for those living with diabetes and CKD.
Ultimately, this pivotal study opens an important window into the future of diabetes management, setting the stage for future inquiries into how best to optimize the therapeutic landscape for patients facing the dual challenges of diabetes and chronic kidney disease. A continued exploration of these emerging trends will contribute significantly to enhancing our understanding and implementation of these crucial treatment modalities in the years to come.
In summary, the temporal analysis of SGLT2 inhibitors and GLP-1 receptor agonists unveils a promising shift in diabetes management, echoing the sentiment of progress toward more holistic and effective treatment paradigms. As the landscape continues to transform, the importance of ongoing research cannot be overstated, as it holds the key to unlocking the full potential of diabetes therapies in improving the quality of life for patients and reversing the trends of diabetes-related morbidity and mortality.
Subject of Research: Prescribing patterns of SGLT2 inhibitors and GLP-1 receptor agonists in patients with chronic kidney disease and type 2 diabetes over time.
Article Title: Temporal Changes in SGLT2 Inhibitor and GLP-1 Receptor Agonist Use in Patients with Chronic Kidney Disease and Type 2 Diabetes, 2012–2023: A US Cohort Study.
Article References: Johannes, C.B., Coleman, C.I., Kovesdy, C.P. et al. Temporal Changes in SGLT2 Inhibitor and GLP-1 Receptor Agonist Use in Patients with Chronic Kidney Disease and Type 2 Diabetes, 2012–2023: A US Cohort Study. Diabetes Ther (2025). https://doi.org/10.1007/s13300-025-01825-5
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s13300-025-01825-5
Keywords: diabetes management, SGLT2 inhibitors, GLP-1 receptor agonists, chronic kidney disease, Type 2 diabetes, patient outcomes, prescribing patterns, treatment trends, nephroprotection, cardiovascular health.
Tags: cardiovascular benefits of diabetes drugsdiabetes management and kidney healthevolving treatment strategies for CKDGLP-1 receptor agonists for diabetes managementimplications of diabetes on renal healthlong-term outcomes of diabetes therapiesnephroprotective effects of SGLT2 inhibitorsprescription patterns of diabetes medicationsresearch on diabetes drug effectivenessSGLT2 inhibitors in chronic kidney diseasetrends in diabetes medication usetype 2 diabetes and kidney disease