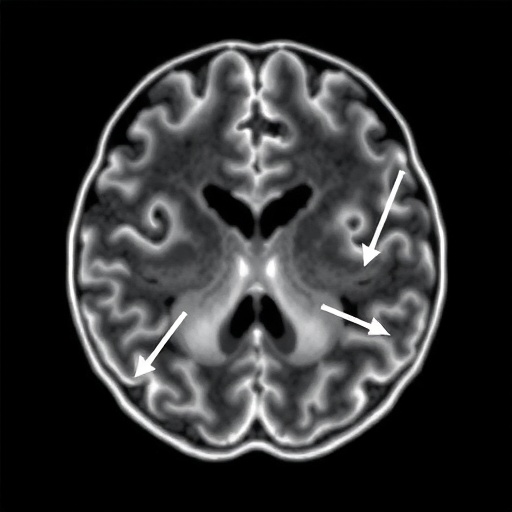
The human brain is a marvel of biological engineering, a labyrinth of neurons fueled by a relentless demand for oxygenated blood, yet for those living with the enigmatic condition known as Moyamoya arteriopathy, this vital supply line is under constant siege. Derived from the Japanese word for a puff of smoke, Moyamoya describes the hazy appearance of fragile collateral vessels that sprout in a desperate attempt to bypass the progressive narrowing of the internal carotid arteries. While the medical community has long understood the structural decay associated with this disease, particularly in pediatric populations, the ability to predict when a catastrophic stroke might occur has remained frustratingly elusive. However, a groundbreaking longitudinal study published in the prestigious journal Pediatric Research has unveiled a predictive frontier that could fundamentally alter how we monitor at-risk patients, shifting the paradigm from reactive management to proactive prevention through the sophisticated use of Transcranial Doppler ultrasound.
The essence of this scientific breakthrough lies in the physiological dynamics of fluid mechanics as applied to the human circulatory system, specifically how blood behaves when forced through increasingly constricted channels. Lead researcher L.R. Sun and their esteemed colleagues began with a compelling hypothesis: that the velocity of blood flow within the brain’s major conduits, measured via non-invasive ultrasound waves, serves as a harbinger of imminent ischemic disaster. By utilizing Transcranial Doppler or TCD technology, the researchers were able to penetrate the temporal windows of the skull to bounce high-frequency sound waves off moving red blood cells, calculating the exact speed at which nutrient-rich blood attempts to navigate the occluded pathways of the Circle of Willis. This study represents a monumental step forward because it moves beyond mere snapshots of anatomical narrowing and enters the realm of real-time hemodynamic stress monitoring, identifying the specific “tipping points” where the brain’s compensatory mechanisms begin to fail.
To understand why this research is sending shockwaves through the neurology and neurosurgery communities, one must first appreciate the staggering complexity of cerebral autoregulation in the face of Moyamoya. As the primary arteries choke off, the brain initiates an angiogenic frenzy, creating a network of tiny, weak vessels that are prone to both leakage and sudden blockage. The researchers found that significantly elevated cerebral blood flow velocities are not merely a symptom of the disease but a loud, acoustic warning sign that the brain is struggling to maintain adequate perfusion against rising resistance. When the flow velocity reaches critical thresholds, it indicates that the pressure gradient is becoming unsustainable, often preceding a transient ischemic attack or a full-blown stroke by weeks or even months. This predictive window is the holy grail of pediatric neurology, offering clinicians a golden hour that spans days, allowing for surgical interventions like encephaloduuroarteriosynangiosis before permanent brain damage occurs.
The methodology employed by Sun and the research team was rigorous, involving a diverse cohort of individuals whose vascular journeys were tracked with meticulous precision over several years. By correlating TCD measurements with the subsequent occurrence of ischemic events, the team established a statistically significant link between specific velocity markers and the clinical outcome of the patients. This is not merely a correlation but a powerful diagnostic tool that translates the invisible physics of turbulent blood flow into a readable map of stroke risk. The study highlights that the higher the velocity recorded in the middle cerebral artery and the internal carotid artery terminus, the more likely the patient was to suffer a future stroke event. This suggests that the turbulent “whooshing” sound of blood forced through a tiny opening is actually the sound of a ticking time bomb, one that can now be timed with unprecedented accuracy.
What makes this discovery particularly viral in the world of medical science is the accessibility and non-invasive nature of the Transcranial Doppler technology itself. Unlike heavily invasive cerebral angiograms that require catheterization and radioactive contrast dyes, or expensive and claustrophobic MRI scans, TCD is a portable, bedside tool that uses simple sound waves to peer into the vascular health of a child or adult. The team’s findings suggest that we can now implement a frequent, low-cost monitoring schedule for Moyamoya patients, identifying those in the “red zone” of stroke risk without subjecting them to the risks of more invasive procedures. This democratization of high-level diagnostic data means that even smaller regional clinics could potentially monitor Moyamoya progression with the same efficacy as major neurological hubs, ensuring that no patient falls through the cracks due to a lack of specialized imaging equipment.
Diving deeper into the technicalities of the study, the researchers observed that it isn’t just the absolute speed of blood but the asymmetry of velocities across the brain’s hemispheres that provides the most definitive clues. In many cases of Moyamoya, the disease progresses unevenly, creating a hemodynamic imbalance that further stresses the fragile “puff of smoke” vessels. The study’s data indicates that when one side of the brain shows a dramatic spike in velocity compared to the other, the risk of a localized stroke or “silent” infarct increases exponentially. This nuanced understanding of intracranial hemodynamics allows for a more personalized approach to medicine, where treatment plans are tailored to the specific flow patterns of an individual’s brain rather than a one-size-fits-all protocol based on general age or symptom presentation.
Furthermore, the implications for the timing of revascularization surgery are profound, as surgeons can now use TCD data to justify earlier intervention in asymptomatic patients who show high-risk flow patterns. In the past, the decision to undergo complex brain surgery was often delayed until the patient showed visible symptoms, which sometimes meant the intervention came too late to prevent some level of cognitive or motor decline. By proving that elevated cerebral blood flow velocity is a reliable precursor to ischemia, Sun and their team have provided a robust justification for preventative surgery. This shift toward “pre-emptive strikes” against Moyamoya has the potential to save thousands of children from the debilitating effects of childhood stroke, preserving their cognitive potential and quality of life for decades to come.
The study also delves into the physiological phenomenon of “steal syndrome,” where the brain’s attempts to redirect blood to oxygen-starved regions actually end up depriving other areas of vital flow. TCD measurements were able to capture these subtle shifts in directionality and speed that occur during high-demand activities or even during changes in blood pressure. The research revealed that patients with higher baseline velocities were much more susceptible to these dangerous fluctuations, essentially living on the edge of a metabolic cliff. By identifying these individuals early, doctors can provide specific lifestyle and medical guidance, such as maintaining strict hydration and blood pressure control, to stabilize the fragile cerebral environment while preparing for a more permanent surgical solution.
One cannot overstate the emotional and psychological impact this research has on the families of those diagnosed with Moyamoya arteriopathy. For parents of children with this condition, every day is shrouded in a cloud of uncertainty, never knowing if a simple bout of crying or a minor illness might trigger a life-altering stroke. The findings of this study offer a sense of agency and control, providing a tangible metric that can be tracked over time. Knowing that a routine ultrasound can signal the need for intervention before a crisis begins provides a level of peace that was previously unavailable. The viral nature of this story stems from this intersection of high-end vascular physics and the deeply human story of protecting the most vulnerable members of society from a silent and invisible predator within their own bodies.
In the context of the broader medical literature, this study bridges a critical gap between theoretical vascular biology and clinical practice. While previous researchers had toyed with the idea of TCD as a monitoring tool, the Sun et al. study is one of the first to provide the long-term, high-quality data necessary to make this a standard of care. The statistical power of their longitudinal approach lends a level of credibility that will likely influence international guidelines for Moyamoya management in the coming years. As we move toward an era of precision medicine, the ability to use a patient’s own hemodynamic profile to predict future events is a prime example of how data-driven insights are outperforming traditional diagnostic snapshots. The research creates a roadmap for future studies to refine these velocity thresholds even further, perhaps even integrating artificial intelligence to analyze TCD waveforms for even more subtle indicators of vascular distress.
Technically speaking, the study utilized mean flow velocities and pulsatility indices to create a multi-dimensional view of the cerebral landscape. The pulsatility index, which measures the resistance to blood flow within the vessel, was found to be a crucial secondary marker that, when combined with high velocity, predicted a nearly certain ischemic event in high-risk groups. This dual-marker system allows for a sophistication in diagnosis that goes beyond simple speed limits; it looks at the “quality” of the flow—whether it is smooth and lamellar or turbulent and strained. The researchers’ ability to synthesize these complex fluid dynamics into a clear predictive model is a testament to the multidisciplinary approach required in modern neuroscience, combining the skills of sonographers, neurologists, and statisticians to solve a singular, deadly problem.
As the scientific community digests these findings, the conversation is already shifting toward how to integrate TCD training more broadly across pediatric clinics. The simplicity of the hardware belies the skill required to accurately locate and sample the deep arteries of the brain, a challenge that this study addresses by advocating for standardized protocols. By showing exactly which vessels provide the most predictive power—namely the terminal ICA and the proximal MCA—the researchers have simplified the task for future technicians, focusing their efforts on the areas that provide the highest “signal” for stroke risk. This focus on practical, actionable data is what ensures that this research won’t just sit in a journal but will actually change the way medicine is practiced in hospitals around the world.
The long-term vision sparked by this study is a world where Moyamoya is no longer a “silent” disease but one that speaks clearly through the medium of ultrasound. We are looking at a future where every child diagnosed with vascular narrowing undergoes regular “acoustic check-ups,” where their brain’s health is measured in centimeters per second. The viral spread of this news is a signal of hope, a testament to the power of human ingenuity to listen to the body’s internal whispers before they turn into screams. By capturing the subtle sounds of blood struggling through narrowed channels, the team led by Sun has given us a stethoscope for the soul’s engine, allowing us to intervene in the clockwork of a stroke before the hands reach midnight.
Ultimately, the study titled “Transcranial Doppler is associated with future ischemic events in moyamoya arteriopathy” is a beacon of progress in the fight against pediatric stroke. It reinforces the idea that the brain is not a black box but a dynamic system that follows the laws of physics—laws that we can now observe and measure to our advantage. As we continue to refine these techniques, the “puff of smoke” that once defined this disease will hopefully dissipate, replaced by the clear and steady flow of blood that every human being deserves. This research is not just a scientific milestone; it is a promise to every family facing a Moyamoya diagnosis that science is listening, and we are finally learning how to hear the warning signs that were right in front of us all along.
Subject of Research: The use of Transcranial Doppler (TCD) ultrasound to predict future ischemic events and stroke risk in patients with Moyamoya arteriopathy by measuring cerebral blood flow velocities.
Article Title: Transcranial Doppler is associated with future ischemic events in moyamoya arteriopathy
Article References: Sun, L.R., Gatti, J.R., Ahmad, S.A. et al. Transcranial Doppler is associated with future ischemic events in moyamoya arteriopathy. Pediatr Res (2026). https://doi.org/10.1038/s41390-026-04827-6
Image Credits: AI Generated
DOI: February 13, 2026
Keywords: Moyamoya Arteriopathy, Transcranial Doppler, Cerebral Blood Flow Velocity, Pediatric Stroke, Ischemic Events, Neurology, Hemodynamics, Stroke Prediction, Medical Ultrasound, Pediatric Research.
Tags: blood flow dynamics in Moyamoyacerebrovascular health monitoringcollateral vessel formation in Moyamoyafluid mechanics in circulatory systeminnovative stroke risk assessmentinternal carotid artery narrowinglongitudinal study on stroke riskMoyamoya arteriopathy stroke riskMoyamoya disease management techniquespediatric stroke predictionproactive stroke prevention strategiesTranscranial Doppler ultrasound