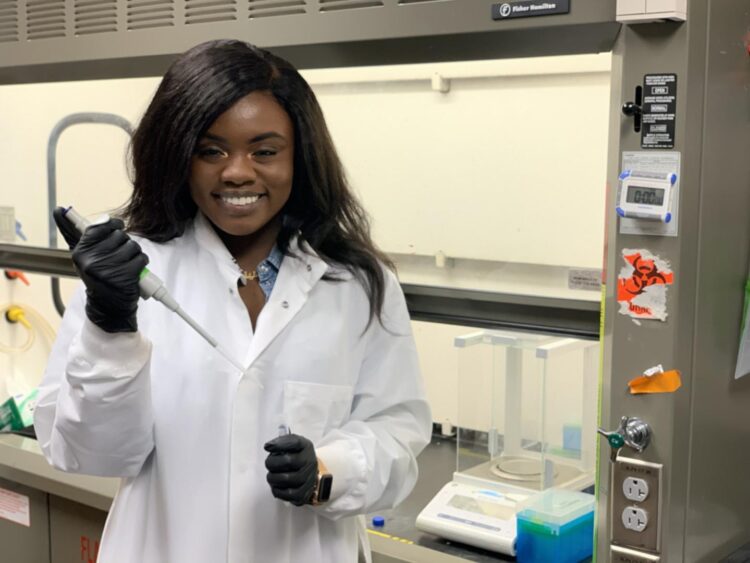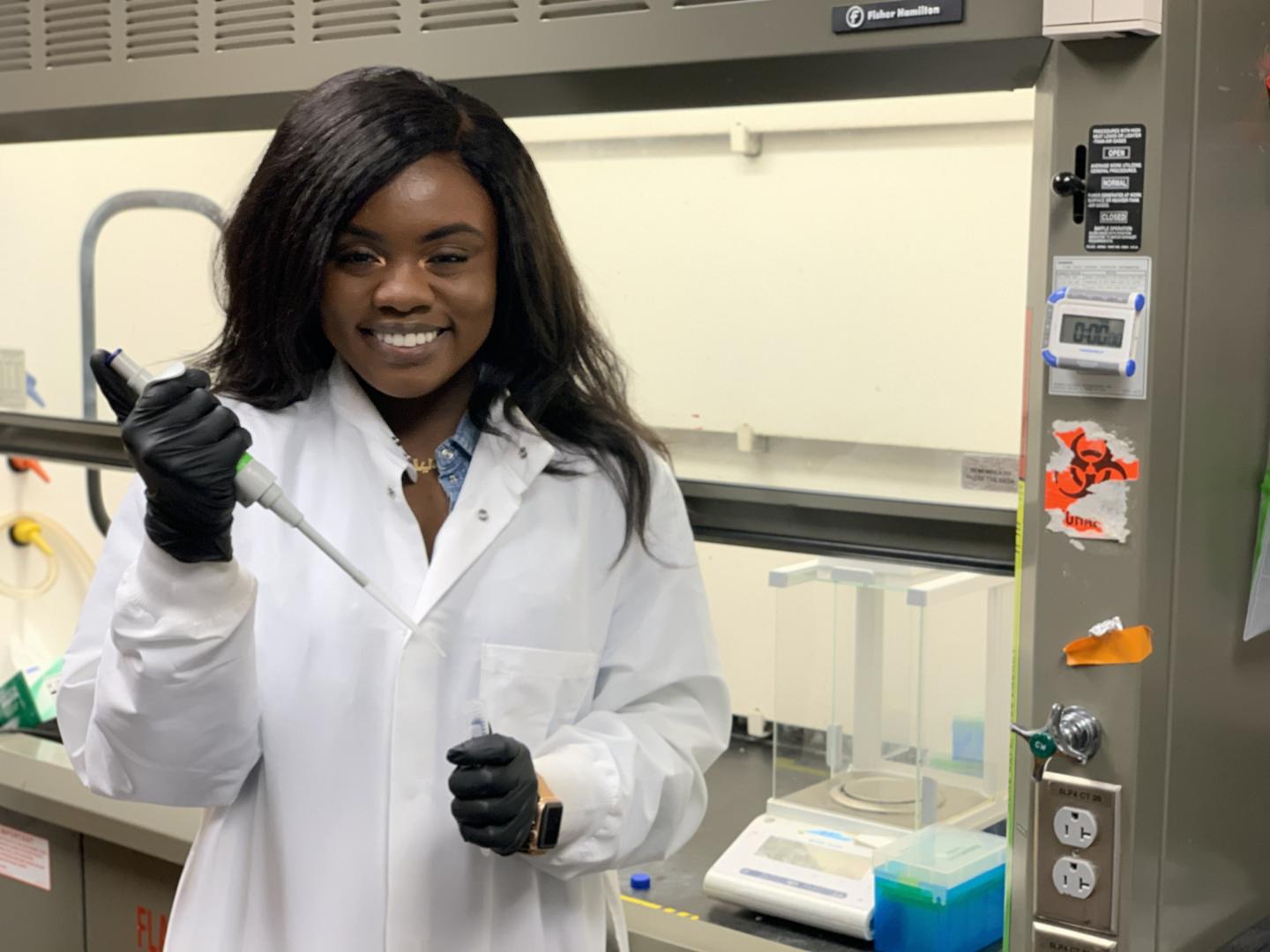
Credit: The University of Texas at Austin
Viruses attack the body by sending their genetic code — DNA and RNA — into cells and multiplying. A promising class of therapeutics that uses synthetic nucleic acids to target and shut down specific, harmful genes and prevent viruses from spreading is gaining steam.
However, only a handful of siRNA, or other RNA interference-based therapeutics have been approved. One of the main problems is getting the siRNA into the body and guiding it to the target.
Chemical engineering researchers in the Cockrell School of Engineering aim to solve that problem, while improving the targeting effectiveness of siRNA. In a new paper in the Journal of Controlled Release, the researchers created several different types of nanoparticles and analyzed them for the ability to deliver and protect siRNA from the body’s immune system.
“The human body is such a diverse place with so many systems to protect us from foreign materials,” said Aaliyah Shodeinde, a fourth-year graduate researcher in the McKetta Department of Chemical Engineering working in professor and drug delivery pioneer Nicholas Peppas’ lab. “So, whenever you try to introduce a synthetically derived material, it almost immediately activates the immune system’s defenses, so you need some kind of protection for the siRNA.”
Several different types of nanoparticles created in Peppas’ lab proved effective at siRNA delivery. The research team measured how well the particles can take in stimuli from their environment, such as changing levels of pH, and adjust accordingly without breaking down.
The team sought to find the right balance between protection and effectiveness of the siRNAs in silencing harmful genes while also minimizing the toxicity of the particles.
“Researchers need to keep in mind that a perfect system may not be feasible at this time because of the need to find a balance with so many moving parts,” Shodeinde said. “What we’ve been able to achieve successfully is modulating so many different parameters to find that sweet spot.”
siRNA is so exciting to researchers because it can be fine-tuned to hinder many different kinds of genes in the body. They then specifically target the mRNA — short for messenger RNA — that tell cells what to do. mRNA has become a part of the popular lexicon lately because several of the COVID-19 vaccines use mRNA to tell cells to produce antibodies to fight off the coronavirus spike proteins.
Shodeinde notes that symptoms in many diseases come from the over- or under-production of proteins. siRNA can be configured to find genes enabling this irregular protein production and, more or less, shut them down. This “upstream” solution is something that traditional therapies can’t achieve, Shodeinde said.
“siRNAs come in before the protein expression level, so we’re hoping that using them to alter the gene expression levels can give us better results,” she said.
This work builds on several previous papers that have come out of Peppas’ lab focused on developing hydrogels and nanoparticles for drug delivery. Just last week Peppas, Shodeinde and Deidra Ward, a chemical engineering Ph.D. student, published a new paper about this in Advanced Healthcare Materials. In it, the authors discuss their vision for the future of RNA-based therapeutics in the treatment of certain types of cancers.
“The results of this new research from our laboratories are promising and add on to our previous research on siRNA delivery that commenced about 10 years ago and has led to about 15 refereed publications and two issued U.S. patents,” said Peppas, the principal investigator of the siRNA paper.
Up next, the researchers want to improve cell targeting. It is key, Shodeinde said, to making sure the siRNAs only interact with target cells and don’t shut down anything they’re not supposed to.
###
The research was funded through grants from the National Institutes of Health. Peppas, who is a professor in the Cockrell School’s McKetta Department of Chemical Engineering and Department of Biomedical Engineering and holds appointments in UT’s College of Pharmacy and the Dell Medical School, is the corresponding author. Other authors include Hannah Hodges, an incoming medical student at UT Southwestern and 2021 graduate of the McKetta Department of Chemical Engineering, as well as David W. Beckman and Bryan Luu, also graduates of the McKetta Department of Chemical Engineering who are now students in medical school.
Media Contact
Nat Levy
[email protected]
Original Source
http://www.
Related Journal Article
http://dx.