A decline in the number of heart patients undergoing unnecessary PCI (angioplasty) procedures reflects improvements in clinical decision-making and documentation to determine which patients benefit most from the procedure, according to new findings by Yale School of Medicine researchers.
The study, which examines how clinical practice has changed since the release of appropriate use criteria, is published in the Nov. 9 issue of Journal of the American Medical Association.
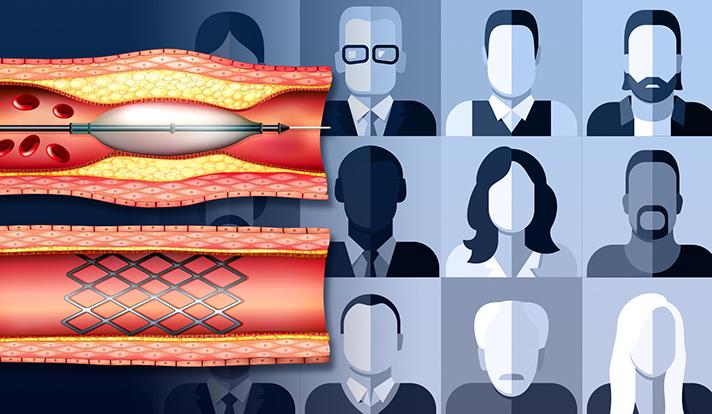
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a non-surgical procedure widely used to treat clogged arteries associated with coronary heart disease. Clinicians, insurers, and policy makers have paid close attention to whether or not patients should undergo PCI, and the procedure has been the focus of national quality improvements initiatives. In 2009, professional medical societies released Appropriate Use Criteria for Coronary Revascularization, which was intended to improve patient selection for PCI and coronary artery bypass grafting.
Past studies found that a large number of elective (non-acute) PCI procedures were classified as "inappropriate," indicating that it was unlikely that the benefits of the procedure would outweigh the risks.
"While the proportion of non-acute PCIs classified as inappropriate has declined, there is still hospital-level variation in inappropriate PCI," said senior author Jeptha P. Curtis, M.D., associate professor of medicine at Yale School of Medicine. "At better-performing hospitals, less than 6% of procedures were classified as inappropriate. In contrast, at worse-performing hospitals, more than 22% of procedures were classified as inappropriate
Curtis and his team analyzed data from the American College of Cardiology's CathPCI Registry to examine the appropriateness of more than 2.7 million PCI procedures performed at 766 hospitals between July 2009 and December 2014.
The team found that the proportion of non-acute PCIs classified as inappropriate decreased from 26% in 2010 to 13% in 2014. The number of acute PCIs performed remained stable, but the volume of non-acute PCIs decreased 34%. Higher proportions of patients undergoing non-acute PCI in 2014 were reported to have severe angina, and more aggressive medical therapy compared with similar patients treated in 2010.
Curtis said the reductions in inappropriate PCI appeared to accelerate in 2011, which coincided with the publication of a high-profile report on PCI appropriateness, and the launch of national performance improvement campaigns.
"These findings suggest the need for ongoing performance-improvement initiatives and hospital benchmarking," said first author Nihar R. Desai, M.D., assistant professor of medicine at Yale School of Medicine. "Our future research will focus on the organizational strategies and structures most strongly associated with lower rates of inappropriate PCI."
###
Other authors on the study included Steven M. Bradley, M.D., Craig S. Parzynski, Brahmajee K. Nallamothu, M.D., Paul S. Chan, M.D., John A. Spertus, M.D., Manesh R. Patel, M.D., Jeremy Ader, Aaron Soufer, M.D., and Harlan M. Krumholz, M.D.
The study was funded by the Agency for Healthcare Research and Quality, A Career Development Award from the Veterans Affairs Health Services Research and Development, the Center for Cardiovascular Outcomes Research at Yale, the National Heart, Lung, and Blood Institute, the National Cardiovascular Data Registry, and the American College of Cardiology.
Citation: JAMA Nov. 9, 2015 doi:10.1001/jama.2015.13764