PHILADELPHIA – A gene encoding a protein linked to tau production—tripartite motif protein 11 (TRIM11)—was found to suppress deterioration in small animal models of neurodegenerative diseases similar to Alzheimer’s disease (AD), while improving cognitive and motor abilities, according to new research from the Perelman School of Medicine at the University of Pennsylvania. Additionally, TRIM11 was identified as playing a key role in removing the protein tangles that cause neurodegenerative diseases, like AD. The findings are published today in Science.
Credit: Penn Medicine
PHILADELPHIA – A gene encoding a protein linked to tau production—tripartite motif protein 11 (TRIM11)—was found to suppress deterioration in small animal models of neurodegenerative diseases similar to Alzheimer’s disease (AD), while improving cognitive and motor abilities, according to new research from the Perelman School of Medicine at the University of Pennsylvania. Additionally, TRIM11 was identified as playing a key role in removing the protein tangles that cause neurodegenerative diseases, like AD. The findings are published today in Science.
AD is the most common cause of dementia in older adults, with an estimated 6 million Americans currently living with the disease. It is a progressive brain disorder that slowly destroys memory and thinking skills. Foundational research at Penn Medicine led by Virginia M.Y. Lee, PhD, the John H. Ware III Professor in Alzheimer’s Research in Pathology and Laboratory Medicine, and the late John Q. Trojanowski, MD, PhD, a former professor of Geriatric Medicine and Gerontology in Pathology and Laboratory Medicine, reveals that one of the underlying causes of neurodegenerative diseases is neurofibrillary tangles (NFTs) of tau proteins, which cause the death of neurons, leading to the symptoms of AD, like loss of memory.
In addition to AD, aggregation of tau proteins into NFTs is associated with over 20 other dementias and movement disorders including progressive supranuclear palsy, Pick’s disease, and chronic traumatic encephalopathy, collectively known as tauopathies. Nevertheless, how and why tau proteins clump together and form the fibrillar aggregates that make up NFTs in patients with these diseases remains unclear. This major gap in knowledge has made the development of effective therapies challenging for researchers.
“Most organisms have protein quality control systems that remove defective proteins, and prevent the mis-folding and accumulation of tangles—like the ones we see with tau proteins in the brain of those with taupathies— but until now we didn’t know how this works in humans, or why it malfunctions in some individuals and not others,” said senior author, Xiaolu Yang, PhD, a professor of Cancer Biology at Penn. “For the first time, we have identified the gene that oversees tau function, and have a promising target for developing treatments to prevent and slow the progression of Alzheimer’s disease and other related disorders.”
Yang and his team, including first author Zi-Yang Zhang, PhD, a postdoctoral researcher in Yang’s lab, previously found that TRIM proteins play an important role in protein quality control in animal cells. After examining over 70 human TRIMs, they found that TRIM11 has a major role in suppressing tau aggregation. TRIM11 possesses three main functions related to the quality control of tau proteins. First, it binds to tau proteins, especially the mutant variants that cause disease, and helps eliminate them. Second, it acts as a “chaperone” for tau, preventing the proteins from mis-folding. Finally, TRIM11 dissolves pre-existing tau aggregates.
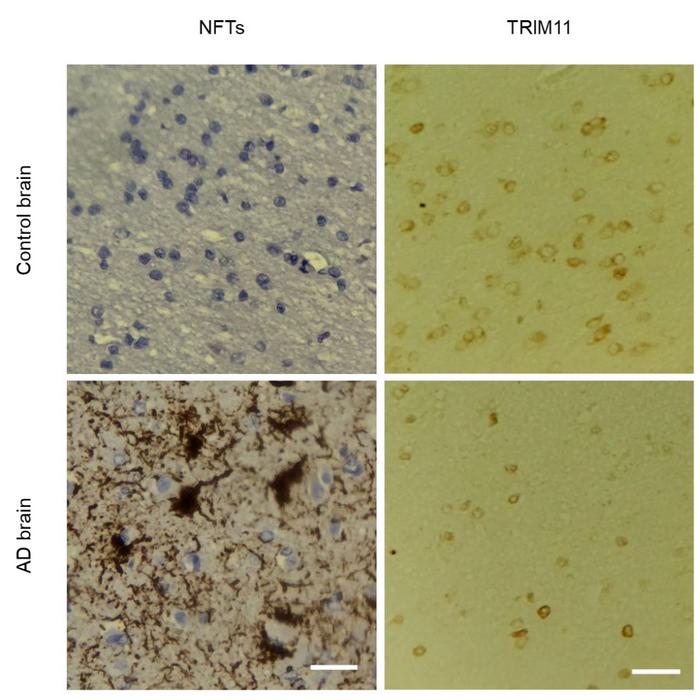
Using postmortem brain tissues of 23 individuals with AD and 14 health controls from the Center for Neurodegenerative Disease Research tissue bank—created and maintained by Lee and Trojanowski—researchers validated these findings, and found that levels of TRIM11 protein are substantially reduced in the brains of individuals with AD, compared to healthy control individuals.
To determine the potential utility of TRIM11 as a therapeutic agent, researchers used adeno-associated viral vector (AAV), a tool commonly used in gene therapy, to deliver the TRIM11 gene into the brain of multiple mouse models. Researchers found that mice with tau pathologies receiving the TRIM11 gene exhibited a marked decrease in the development and accumulation of NFTs, and had much improved cognitive and motor abilities.
“Not only do these findings tell us that TRIM11 could play an important role in protecting people from Alzheimer’s and similar diseases, but we also see that we might be able to develop future therapies that replenish TRIM11 in individuals with lower levels,” said Yang. “We are eager to work with our colleagues to explore the possibility of developing gene therapies that halt the progression of neurodegenerative disease.”
This study was supported by the National Institutes of Health (R01CA243520, UL1TR000003) and funding received by Penn under a sponsored research agreement with Wealth Strategy Holding Limited.
Editor’s note: Yang is an inventor on patents and patent applications owned by the University of Pennsylvania related to TRIM proteins, and is a co-founder and equity holder of Evergreen Therapeutics LLC, which received investments from Wealth Strategy Holding Limited. Penn and Yang have either received, or may receive in the future, financial consideration related to the licensing of certain Penn intellectual property to Evergreen Therapeutics LLC.
###
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, excellence in patient care, and community service. The organization consists of the University of Pennsylvania Health System and Penn’s Raymond and Ruth Perelman School of Medicine, founded in 1765 as the nation’s first medical school.
The Perelman School of Medicine is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $550 million awarded in the 2022 fiscal year. Home to a proud history of “firsts” in medicine, Penn Medicine teams have pioneered discoveries and innovations that have shaped modern medicine, including recent breakthroughs such as CAR T cell therapy for cancer and the mRNA technology used in COVID-19 vaccines.
The University of Pennsylvania Health System’s patient care facilities stretch from the Susquehanna River in Pennsylvania to the New Jersey shore. These include the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Chester County Hospital, Lancaster General Health, Penn Medicine Princeton Health, and Pennsylvania Hospital—the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is an $11.1 billion enterprise powered by more than 49,000 talented faculty and staff.
Journal
Science
DOI
10.1126/science.add6696
Method of Research
Randomized controlled/clinical trial
Subject of Research
Animals
Article Title
TRIM11 protects against tauopathies and is down-regulated in Alzheimer’s disease
Article Publication Date
28-Jul-2023
COI Statement
Yang is an inventor on patents and patent applications owned by the University of Pennsylvania related to TRIM proteins, and is a co-founder and equity holder of Evergreen Therapeutics LLC, which received investments from Wealth Strategy Holding Limited. Penn and Yang have either received, or may receive in the future, financial consideration related to the licensing of certain Penn intellectual property to Evergreen Therapeutics LLC.




