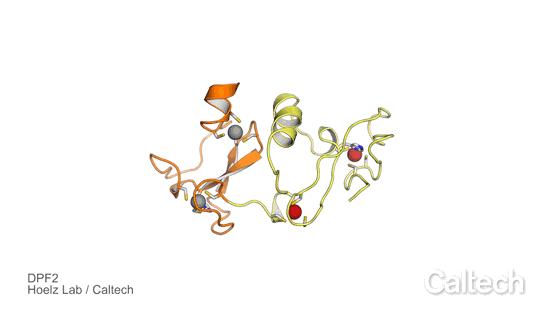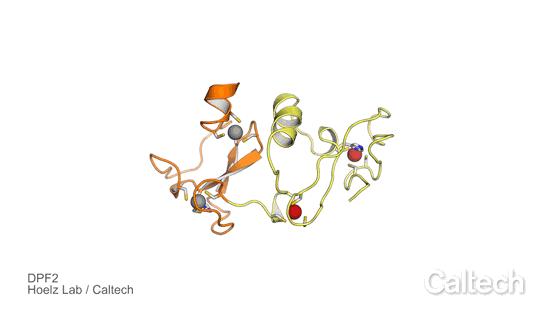
Credit: Hoelz Lab/Caltech
Many things go wrong in cells during the development of cancer. At the heart of the chaos are often genetic switches that control the production of new cells. In a particularly aggressive form of leukemia, called acute myeloid leukemia, a genetic switch that regulates the maturation of blood stem cells into red and white blood cells goes awry. Normally, this switch leads to appropriate numbers of white and red blood cells. But patients with acute myeloid leukemia end up with a dangerous accumulation of blood stem cells and a lack of red and white blood cells — cells that are needed to supply the body with oxygen and fight infections.
Now, researchers at Caltech and the Sylvester Comprehensive Cancer Center at the University of Miami are narrowing in on a protein that helps control this genetic switch. In healthy individuals, the protein, called DPF2, stops the production of red and white blood cells when they do not need to be replaced. That is, it turns the switch off. But the protein can be overproduced in acute myeloid leukemia patients. The protein basically sits on the switch, preventing it from turning back on to make the blood cells as needed. Patients who overproduce DPF2 have a particularly poor prognosis.
In a new study, to be published the week of May 22, 2017, in the journal Proceedings of the National Academy of Sciences, the researchers demonstrate new ways to impede DPF2, potentially rendering acute myeloid leukemia more treatable. They report new structural and functional details about a fragment of DPF2. This new information reveals targets for the development of drugs that would block the protein's function.
"Many human diseases, including cancers, arise because of malfunctioning genetic switches," says André Hoelz, the corresponding author of the study. Hoelz is a professor of chemistry at Caltech, a Heritage Medical Research Institute (HMRI) Investigator, and a Howard Hughes Medical Institute (HHMI) Faculty Scholar. "Elucidating how they work at atomic detail allows us to begin the process of custom tailoring drugs to inactivate them and in many cases that is a significant step towards a cure."
Red and white blood cells are constantly regenerated from blood stem cells, which reside in our bone marrow. Like other stem cells, blood stem cells can live forever. It is only when they become differentiated into specific cell types, such as red and white blood cells, that they then become mortal, or acquire the ability to die after a certain period of time.
"Our bodies use a complex series of genetic switches to differentiate a blood stem cell into many different cell types. These differentiated cells then circulate in the blood and serve a variety of different functions. When these cells reach the end of their lifespan they need to be replaced," says Hoelz. "This is somewhat like replacing used tires on a car."
To investigate the role of DPF2 and learn more about how it controls the genetic switch for making blood cells, the Hoelz group partnered with Stephen D. Nimer, co-corresponding author of the paper and director of the Sylvester Comprehensive Cancer Center, and his team. First, Ferdinand Huber and Andrew Davenport — both graduate students at Caltech in the Hoelz group and co-first-authors of the new study–obtained crystals of a portion of the DPF2 protein containing a domain known as a PHD finger, which stands for planet homeodomain. They then used X-ray crystallography, a process that involves exposing protein crystals to high-energy X-rays, to solve the structure of the PHD finger domain. The technique was performed at the Stanford Synchrotron Radiation Lightsource, using a dedicated beamline of Caltech's Molecular Observatory.
The results revealed how DPF2 binds to a DNA-protein complex, called the nucleosome, to block the production of red and white blood cells. The protein "reads" various signals displayed on the nucleosome surface by adopting a shape that fits various modifications on the nucleosome complex, like the different shaped pieces of a jigsaw puzzle. Once the protein binds to this DNA locus, DPF2 turns off the switch that regulates blood cell differentiation.
The next step was to see if DPF2 could be blocked in human blood stem cells in the lab. Sarah Greenblatt, a postdoctoral associate in Nimer's group and co-first author of the study, used the structural information from Hoelz's group to create a mutated version of the protein. The Nimer group then introduced the mutated protein in blood stem cells, and found that the mutated DPF2 could no longer bind to the nucleosome. In other words, DPF2 could no longer inactivate the switch for making blood cells.
"The mutated DPF2 was unable to bind to specific regions in the genome and could not halt blood stem cell differentiation," says Huber. "Whether DPF2 can also be blocked in the cancer patients themselves remains to be seen." The researchers say a structural socket in DPF2, one of the puzzle-piece-like regions identified in the new study, is a good target for candidate drugs.
###
The study, titled "Histone-Binding of DPF2 Mediates Its Repressive Role in Myeloid Differentiation," was funded by a PhD fellowship of the Boehringer Ingelheim Fonds, a National Institutes of Health Research Service Award, the National Cancer Institute of the National Institutes of Health, a Faculty Scholar Award of the Howard Hughes Medical Research Institute, the Heritage Medical Research Institute, Caltech startup funds, the Albert Wyrick V Scholar Award of the V Foundation for Cancer Research, a Kimmel Scholar Award of the Sidney Kimmel Foundation for Cancer Research, and a Teacher-Scholar Award of the Camille & Henry Dreyfus Foundation. Other authors are Concepcion Martinez and Ye Xu of the University of Miami and Ly P. Vu of the Memorial Sloan Kettering Cancer Center.
Media Contact
Whitney Clavin
[email protected]
626-395-1856
@caltech
http://www.caltech.edu
############
Story Source: Materials provided by Scienmag