In a groundbreaking study poised to redefine our understanding of type 1 diabetes (T1D) pathogenesis in children, researchers have illuminated a complex immunological imbalance involving stem-like and effector T cell populations. This imbalance is evident not only in conventional T cells but also across regulatory T cell subsets, pointing to a nuanced dysregulation of immune homeostasis during the earliest stages of T1D development. The implications of these findings extend far beyond descriptive immunology, offering new mechanistic insights into how immune tolerance collapses and how targeted therapies might be devised to restore balance and halt disease progression.
Type 1 diabetes is characterized by autoimmune destruction of pancreatic β-cells, leading to lifelong insulin dependence and severe metabolic dysregulation. While extensive research has established the central role of autoreactive T cells in targeting islet antigens, the detailed cellular states and their shifts during early disease onset have remained elusive. Niederlova et al. employed state-of-the-art single-cell transcriptomic and immunophenotyping techniques to dissect the T cell compartment in pediatric patients newly diagnosed with T1D. This high-resolution approach enabled the team to identify distinct stem-like and effector T cell profiles, challenging the traditional binary view of T cell differentiation and function in autoimmunity.
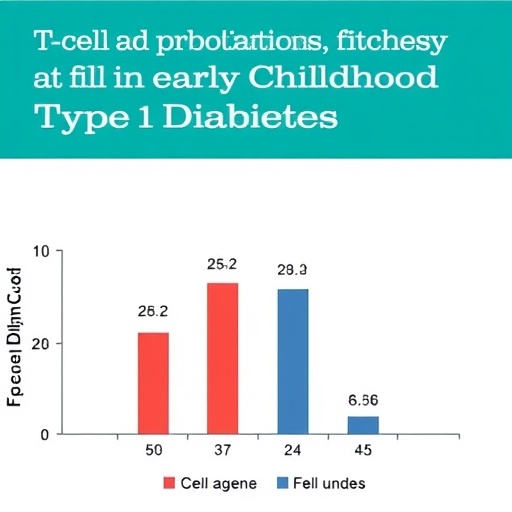
What sets this study apart is the emphasis on stem-like T cells, a subset previously recognized primarily in chronic infections and cancer immunology for their self-renewal and multipotent capabilities. These cells serve as a reservoir, capable of replenishing exhausted effector populations. Intriguingly, in children with early T1D, the researchers observed a significant skewing in the ratio of stem-like to effector T cells. Rather than maintaining a dynamic equilibrium, this balance was disrupted, favoring an effector-dominant response that fuels autoimmune attack while depleting the regenerative stem-like pool. This shift may contribute to the relentless progression of β-cell destruction seen in early disease stages.
Furthermore, this alteration was not restricted to conventional T cells; regulatory T cells (Tregs), which are critical for maintaining immune tolerance, exhibited a similar imbalance. Regulatory subsets failed to maintain their stem-like state, which is crucial for their suppressive functions, thereby potentially diminishing their capacity to restrain autoreactive effector cells. This finding underscores a dual breakdown in immune regulation—both in the generation of aggressive effector clones and the loss of effective regulatory control.
At the molecular level, the study delved into transcriptional programs governing these states. Stem-like T cells were characterized by high expression of genes associated with self-renewal, quiescence, and multipotency, including TCF7 and LEF1. In contrast, effector populations upregulated cytotoxic and inflammatory genes such as GZMB and IFNG, indicating an activated, tissue-destructive phenotype. What is particularly compelling is that the transition from stem-like to effector states appeared accelerated in T1D patients, suggesting that autoimmune conditions may prematurely exhaust progenitor T cell pools, pushing the immune system toward a terminal, pathogenic state.
The implications for therapeutic intervention are profound. Current immunomodulatory strategies often aim to broadly suppress immune activation, risking systemic immunosuppression and attendant complications. Understanding the stem-like/effector dynamics opens avenues for more precise interventions designed to preserve or restore stem-like T cell populations while recalibrating effector responses. Strategies such as promoting stem-like T cell maintenance, enhancing Treg function, or selectively targeting pathogenic effector subsets could revolutionize early-stage T1D treatment.
Notably, the researchers highlight the importance of temporal dynamics. Longitudinal sampling suggested that the imbalance intensifies rapidly soon after clinical onset, indicating a narrow therapeutic window. Early intervention that can modulate these T cell states before irreversible β-cell loss occurs could dramatically alter disease trajectories, potentially delaying or preventing full-blown diabetes.
This study also contributes to a broader paradigm in immunology, illustrating the significance of stem-like memory T cells in autoimmune diseases beyond the established contexts of infection and malignancy. The concept that autoimmunity reflects, at least in part, the exhaustion and misdirection of a regenerative immune compartment offers a fresh lens through which to examine a host of chronic, immune-mediated conditions.
Moreover, the integration of conventional and regulatory T cell analysis embodies a holistic approach to immune dysregulation, moving beyond isolated cell populations to capture system-wide immune architecture alterations. This systemic perspective is essential to fully appreciate the interconnected pathways that drive autoimmunity and to design treatments that restore balance rather than simply dampen immune responses.
Technically, the study’s use of high-throughput single-cell RNA sequencing combined with advanced computational clustering algorithms allowed for unprecedented resolution of T cell heterogeneity. The application of trajectory inference and pseudotime analyses provided powerful insight into differentiation pathways, enabling the mapping of T cell states as a continuum rather than discrete categories. This methodological innovation sets a new standard for immunophenotyping in autoimmune research.
Future research directions prompted by this work include exploring the molecular cues that govern the transition between stem-like and effector states, such as cytokine signaling, metabolic pathways, and epigenetic modifications. Elucidating these drivers could identify novel drug targets to modulate T cell fate decisions intentionally. Additionally, expanding this approach to other autoimmune diseases may uncover common immune dysregulation patterns that transcend tissue-specific contexts.
It is also essential to investigate environmental and genetic factors influencing T cell imbalance in T1D. For example, certain HLA alleles may predispose individuals to accelerated depletion of stem-like T cells or aberrant activation of effector populations. Understanding these interactions could pave the way for personalized medicine approaches tailored to an individual’s immunogenetic background.
The translational potential of these findings is underscored by their relevance to emerging cell-based therapies. Stem-like T cells, with their capacity for self-renewal and plasticity, might be harnessed or mimicked in adoptive T cell therapies aimed at restoring immune equilibrium. Conversely, engineering regulatory T cells to maintain or re-establish stem-like characteristics could enhance their durability and suppressive function in autoimmune settings.
Taken together, Niederlova et al.’s research represents a milestone in the quest to decode the immune underpinnings of type 1 diabetes. The detailed characterization of T cell state imbalances and their implications for disease onset and progression offers a powerful new avenue for therapeutic innovation. As the field moves toward precision immunology, findings such as these will be instrumental in shaping the next generation of interventions designed to prevent, delay, or reverse autoimmune diseases in children and beyond.
In conclusion, this study has not only illuminated a previously underappreciated facet of immune dysregulation in pediatric T1D but also set a transformative agenda for the future of autoimmune research and treatment. The sophisticated interplay between stem-like and effector T cells uncovered here invites a reevaluation of how immune memory, tolerance, and activation intersect in health and disease. By harnessing this knowledge, the vision of targeted, effective, and personalized therapies for type 1 diabetes becomes increasingly attainable, promising a new era of hope for patients and clinicians alike.
Subject of Research:
The immunological imbalance of stem-like and effector T cell states in pediatric type 1 diabetes, encompassing both conventional and regulatory T cell subsets.
Article Title:
Imbalance of stem-like and effector T cell states in children with early type 1 diabetes across conventional and regulatory subsets.
Article References:
Niederlova, V., Neuwirth, A., Neuman, V. et al. Imbalance of stem-like and effector T cell states in children with early type 1 diabetes across conventional and regulatory subsets. Nat Commun (2025). https://doi.org/10.1038/s41467-025-66459-4
Image Credits:
AI Generated
Tags: autoimmune destruction of pancreatic β-cellsautoreactive T cells targeting islet antigensearly childhood type 1 diabetes pathogenesiseffector T cell profiles in autoimmunityimmune homeostasis in diabetesimmunophenotyping in diabetes studiesmechanistic insights into immune tolerance collapsepediatric type 1 diabetes researchregulatory T cell subsets dysregulationsingle-cell transcriptomic techniques in immunologyT cell imbalance in type 1 diabetestargeted therapies for type 1 diabetes